In December 2018, the Chan Zuckerberg Initiative (founded by Priscilla Chan and Mark Zuckerberg) committed $51.9M to accelerate research into cures for neurogenerative disease, beginning with the fundamental biology underlying them. Nine teams and 17 early career scientists received funding across a broad spectrum of neurogenerative diseases and research backgrounds
Ethan Lippmann, Ph.D., an assistant professor at Vanderbilt University, is one of only two early career awardees who are engineers. “I believe I received the award because of my expertise in the blood-brain barrier, but also because I often have a technology-driven versus a hypothesis-driven perspective,” Lippmann said. “Sometimes it is more effective to solve a problem by developing a new way to approach it, rather than having an educated guess that may ultimately be incorrect.”
“Sometimes it is more effective to solve a problem by developing a new way to approach it, rather than having an educated guess.”
Focusing on Transport
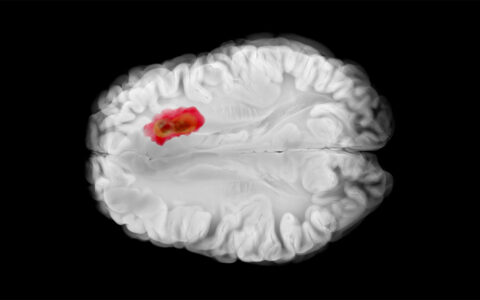
Lippman’s research will help clarify the mechanisms that control vascular transport across the blood-brain barrier, specifically how expression of critical proteins like GLUT1 or P-glycoprotein is regulated in this band of endothelium.
“Dysfunction of the blood-brain barrier is causative or exacerbates nearly every neurodegenerative disorder. Many patients exhibit loss of transport protein expression and activity in diseases such as Alzheimer’s. Understanding why a subset of people might have blood-brain barrier dysfunction is critically important for understanding what happens with these diseases,” Lippmann said.
Building Test Tissues
Lippmann’s lab will use genomic engineering techniques to identify signaling pathways that regulate transporter expression and activity. The team plans to build a working tissue model to explore why expression of genes that control transport is altered in neurodegenerative disease. They will use 3-D biomimetic cultures from induced pluripotent stem cells that mirror the architecture and function of the neurovascular unit.
“Using new 3-D culture technology, we can develop blocks of tissue that have vasculature and neuronal networks. This enables us to run tests we could never run before, in a human system,” Lippmann said.
“We can develop blocks of tissue that have vasculature and neuronal networks. This enables us to run tests we could never run before.”
This modeling process is possible through the work of Sir John B. Gurdon, Ph.D., and Shinya Yamanaka, M.D., who won the Nobel Prize in 2012 for discovering how to make mature cells regress back to pluripotency, resembling the undifferentiated state they had soon after conception. Having “lost their memory,” reprogrammed cells can be sent on a trajectory toward becoming any given cell type.
Lippmann has been figuring out how to make new cell types from these pluripotent stem cells since graduate school. He recently solved one of many thorny issues in reprogramming cell types: in vitro neurons that wouldn’t mature. Lippmann recreated a natural signal found in the brain that facilitates the maturation of these cells. Now, his in vitro neurons fire and link up, enabling him to study signaling and disease progression.
Expanding from in vitro Studies
Once he gains a deeper understanding of transport mechanisms in human tissue models, Lippmann wants to partner with others in the Chan Zuckerberg Initiative network to generate mouse models. The objective will be to see how removing some of the genes that influence expression of transport proteins affects disease progression.
Lippmann also envisions bioinformatic studies to see if there are transport gene variations within the population that increase risk of diseases like Alzheimer’s, or if there are environmental factors that increase susceptibility to losing transporters.
Lippmann’s work also aims at improving drug transport. In neurodegenerative diseases like Parkinson’s, for example, blood-barrier dysfunction is not believed to be causative, but drug delivery across the blood-brain barrier is important for treatment. “The answers to why delivery is enhanced or impaired may dictate how the next generation of drugs is applied,” Lippmann said.