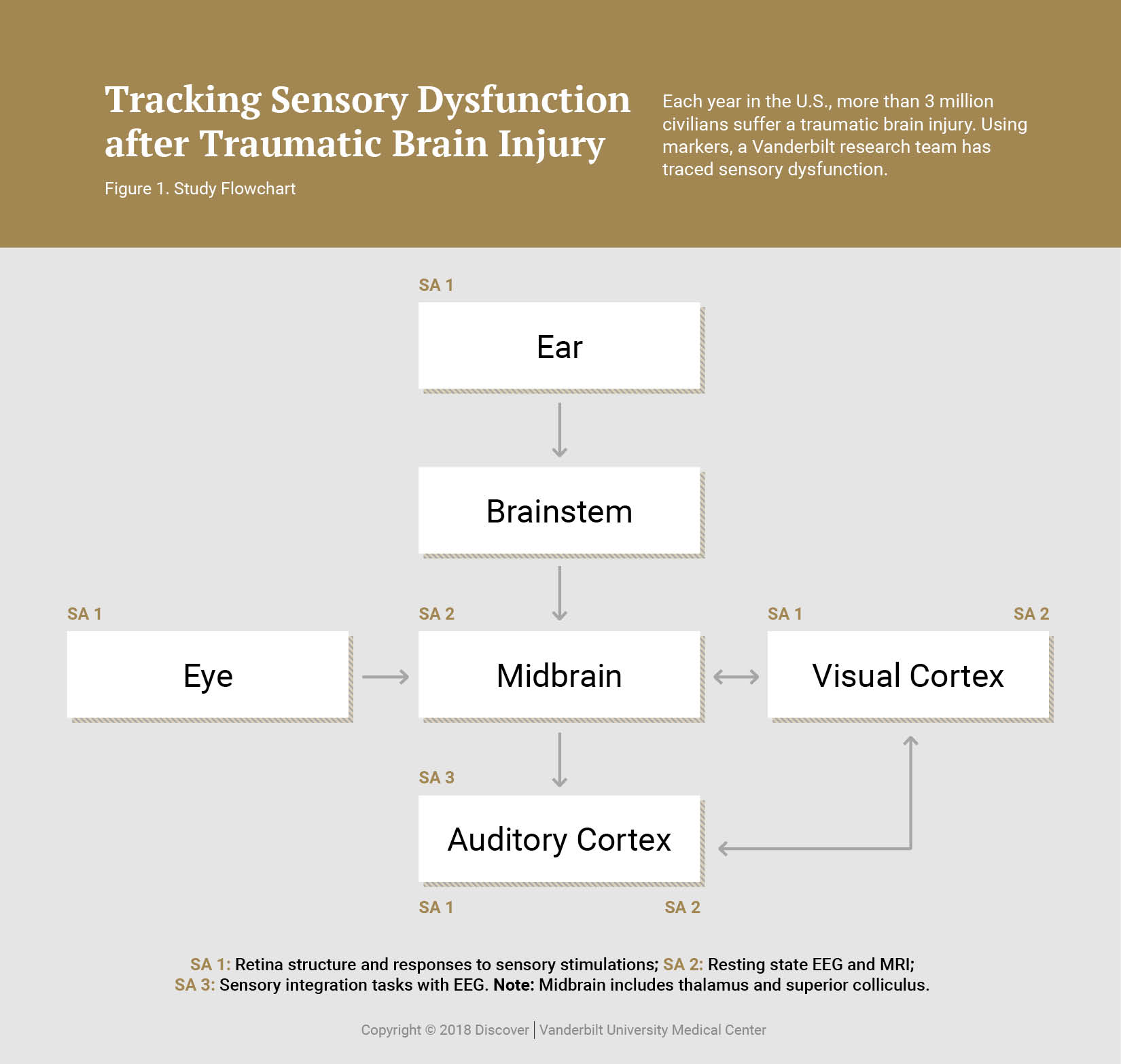
In the United States, 3 million civilians suffer a traumatic brain injury (TBI) annually. TBI is also considered the hallmark injury of the Iraq and Afghanistan wars. While civilians most often incur brain injury from blunt force trauma, veterans typically suffer TBI from improvised explosive devices.
Nearly 75 percent of TBI patients self-report difficulty with vision or hearing, yet a majority pass standard eye and ear exams. These self-reported vision difficulties include light sensitivity, blurred or double vision, and difficulty reading. Hearing difficulties include tinnitus and hearing loss. These sensory impairments are still detectable from months to years after the injury in most affected patients – even in mild TBI patients, who comprise 80 percent of all cases. This sensory dysfunction could potentially arise from peripheral, ocular or cortical damage.
Further, blast patients may have damage to the optic nerve and retina that is not visible until months after injury. Laboratory studies in an animal model suggest that while outer retinal changes either resolve or remain focal, inner retinal changes are more severe and spread to the entire retina. Oxidative stress, neuroinflammation, cell death and vision loss occur days to weeks after injury, indicating ongoing neurodegenerative activity. This decline suggests that the eyes of persons with TBI should be monitored beginning immediately post-injury and continuing for years.
Developing Clinical Markers for TBI-related Retinal Damage
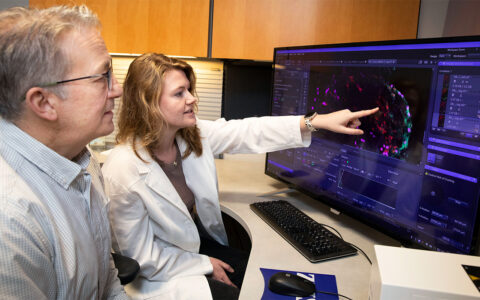
Most visual and auditory dysfunction in TBI patients is self-reported. Clinicians need objective, quantitative clinical markers that can serve as diagnostics for identifying mild brain trauma and its associated sensory dysfunction. Tonia Rex, Ph.D., of Vanderbilt Eye Institute, and her collaborators are focused on the close association of sensory dysfunction and TBI. Rex is the lead investigator on a multi-site study of civilians with blunt-force TBI and active duty service members and veterans with blast-induced TBI, with the goal of developing diagnostic approaches.
The team has already designed an array of assessments and analyses to monitor these markers. These new measures will establish clinically useful tools for accurate diagnosis of TBI patients and provide outcome measures for future clinical trials. The project is a multi-site collaboration among military hospitals, Vanderbilt Eye Institute ophthalmologists and Vanderbilt University engineering faculty.
“We want to make sure we’re running the right tests,” said Rex. “In some cases, veterans have gone undiagnosed because their vision appeared normal on the standard Snellen eye chart – and yet they continued to complain of vision problems. We want to prevent that from happening.”
Future Research
Rex and her team are also testing how neurodegeneration from blast-induced eye trauma is exacerbated by immune response. They are seeking to identify therapeutic interventions to prevent neurodegeneration caused by trauma.
“We’re trying to move the conversation forward on testing requirements and potential therapies for veterans with traumatic eye injury,” said Rex. “These men and women have risked their lives for our country. They should receive the best possible care when they return.”