Previous data have shown that late-life depression (LLD) is associated with cognitive deficits, and that vascular pathology is common in LLD, contributing to changes in cerebral function. However, the underlying relationship between depression and dementia is unclear. Depressed elders tend not to respond as well to antidepressant medications. Moreover, even for individuals who do respond to treatment, data suggest that medications may not stave off depression in the long term.
“We’ve known for quite a while that older adults who are depressed have age-related brain changes that occur faster than should be expected,” said Warren Taylor, M.D., director of Geriatric Psychiatry at Vanderbilt University Medical Center. “As physicians who treat these patients, we need to know whether clinical characteristics could serve as phenotypes that inform risk of subsequent cognitive decline and disability.”
Researching LLD Phenotypes
Phenotypes within LLD have previously been distinguished by late onset depression (LOD) and early onset depression (EOD), typically using a cutoff age between 50 and 60 years. While both EOD and LOD have been associated with increased dementia risk, recent work suggests that individuals with EOD may be particularly at risk. This is thought to be related to the number of depressive episodes throughout their lives, even if they have achieved remission one or more times.
In a longitudinal study, published last fall in the American Journal of Geriatric Psychiatry, Taylor and co-investigators at Vanderbilt; Duke University; the University of Connecticut; and the V.A. Medical Center, Tennessee Valley Healthcare System, followed 273 depressed and 164 never-depressed community dwellers aged 60 years or older for an average of five years. Participants were examined at onset, at antidepressant remission at three months (acute response) and at 12 months (chronic response).
Participants in the study completed annual neuropsychological testing, including self-report questions derived from the National Institute of Mental Health Epidemiological Catchment Area program and the clinician-rated Montgomery-Asberg Depression Rating Scale (MADRS). Neuropsychological measures were grouped into domains of episodic memory, attention-working memory, verbal fluency and executive function.
Results and Conclusions
Depressed participants exhibited poorer performance at baseline and greater subsequent decline in all domains. Individuals with EOD exhibited a greater decline over time in all domains than late-onset or non-depressed groups, supporting the theory that repeated depressive episodes may contribute to decline.
Both groups of patients – those who experienced antidepressant remittance and those who did not – exhibited greater decline in episodic memory and attention-working memory than non-depressed subjects. Three-month remitters also exhibited a greater decline in verbal fluency and executive function, whereas 12-month non-remitters exhibited greater decline in executive function than other groups.
“These clinical characteristics may help us identify older people who are at high risk for decline, so we can follow them more carefully and hopefully intervene earlier,” said Taylor. “We want them to have improved quality of life. We want to help them alleviate stress. But most important, we want to help them make decisions about the future before they lose the ability to do so.”
Improving Geriatric Depression Treatments
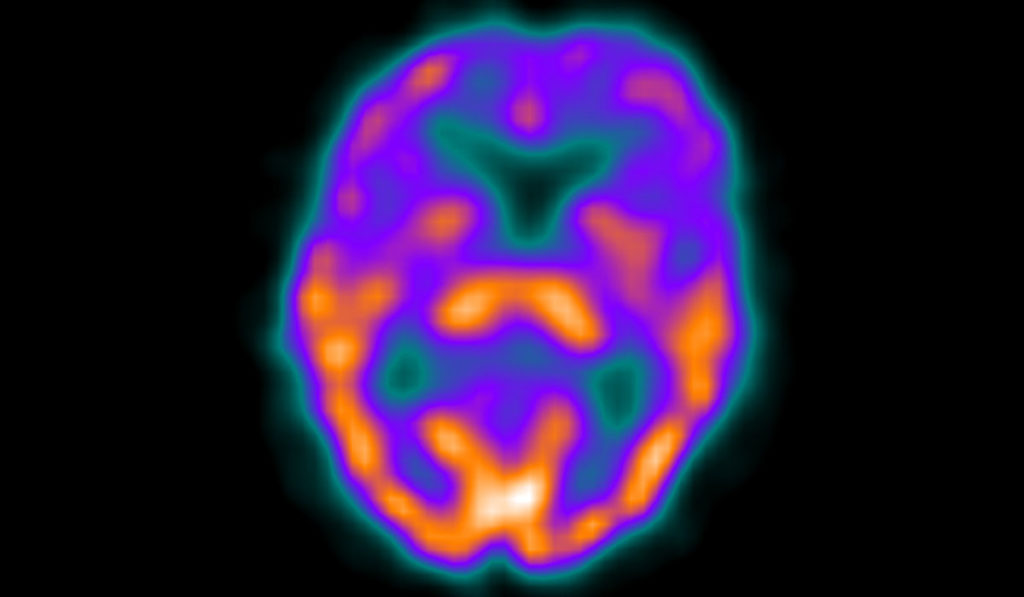
In his research, Taylor combines clinical and neuropsychological evaluations with genetic analyses and advanced neuroimaging techniques. The objective is not only to better elucidate neurobiological contributors to depression but also to examine biomarkers predictive of response to antidepressant medications. His current work proposes to repurpose existing drug compounds that may improve antidepressant responses.
“Depression is so personal and has so many contributing factors. The goal is to find the right intervention, or right combination of interventions, that will help each patient improve.”
“But new medicines are not the only answer,” Taylor said. “We need better treatments for depression across the board. What can we do to improve mood and memory disturbances, in both people who are and are not at high risk for Alzheimer’s? Psychotherapy works well with older adults but it can be expensive and difficult to find a skilled provider. Cognitive remediation is a new approach that shows great promise.”
“Depression is so personal and has so many contributing factors. The goal is to find the right intervention, or right combination of interventions, that will help each patient improve.”