Vanderbilt surgeons are expanding options for lung transplant patients and building on their groundbreaking successes with ex vivo lung perfusion (EVLP).
In 2019, Matthew Bacchetta, M.D., an associate professor of thoracic surgery at Vanderbilt University Medical Center, performed the first successful lung transplant using EVLP. Now, Bacchetta is a principal investigator on a trial designed to increase the number of lungs eligible for the procedure. “We’re trying to find ways to improve the durability and range of interventional capabilities of organ support systems,” he said.
“We’re trying to find ways to improve the durability and range of interventional capabilities of organ support systems.”
Extending the Transplant Window
Ex vivo lung perfusion maintains organs in a homeostatic environment in anticipation of transplant. The procedure extends the transplant window, allowing time for immunomodulation or regenerative therapies that might help rehabilitate a lung and, hopefully, reduce acute rejection rates.
Vanderbilt is one of 14 sites applying EVLP to help extend lung preservation time in the new trial. The study has enrolled 186 participants – all slated to receive orthotopic single or double lung transplants. Vanderbilt is the third largest enroller in the study, Bacchetta said.
Researchers will determine whether or not evaluating lungs for EVLP and performing the procedure pre-transplant increases recipient survival rates six months post-transplant. Other trials are underway worldwide to test whether EVLP can expand the donor pool while maintaining – or improving – outcomes.
The goal is to increase organ availability. “EVLP could help rehabilitate lungs that without it, might be unsuitable for transplant,” Bacchetta said.
“EVLP could help rehabilitate lungs that without it, might be unsuitable for transplant.”
Expanding Technology
Keeping donating organs alive longer helps them reach more patients. It also offers more time to monitor how well an organ is performing before deciding to transplant it, Bacchetta says, and to be more confident of an acceptable match.
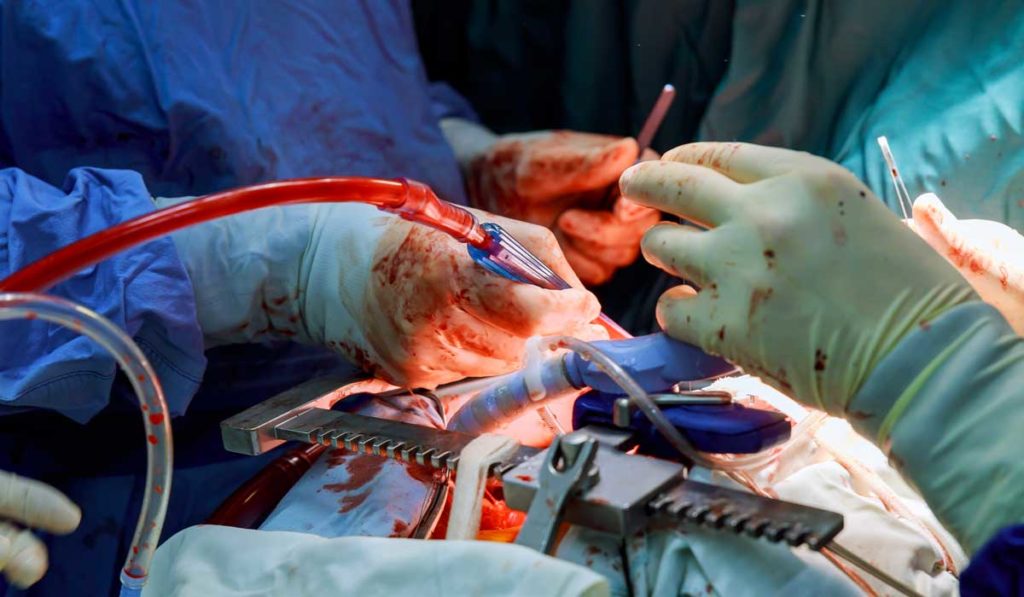
A cross-circulation technique provides an opportunity to further extend the transplant window, according to Bacchetta’s previous research in The Journal of Thoracic and Cardiovascular Surgery. In the proof-of-feasibility study, researchers harvested lungs from pigs, cannulated the pulmonary artery and vein, connected the lungs to recipient pigs’ circulatory systems, and maintained the lungs using EVLP.
The extra-corporeal lung support system was capable of maintaining lung tissue structure and respiratory function for four days. Said Bacchetta, “We report the longest duration of support for ex vivo lungs yet in the literature.”
Moving to the Surgical Suite
Connecting donor lungs to their recipients via cross-circulation helps improve the lung recovery process. Damaged or marginal lungs benefit from nutrients in recipient whole blood and it is a means of getting rid of mounting metabolic waste.
A major difference between the pig study and Bacchetta’s previous EVLP proof-of-concept studies (also performed in pigs) is that lung recipients remained conscious. This approach makes the cross-circulation system far more translational, wrote the authors. “We envision that this system could be applicable in clinical settings to recover and regenerate damaged donor organs, and in translational research settings as a platform to investigate new strategies for lung bioengineering.”
Bacchetta is hopeful the technique will quickly move to the surgical suite for certain patients. “We plan to offer this surgery for patients who are failing medical therapy for pulmonary hypertension,” he said. He also hopes EVLP research will expand to the liver.