In 2016, a new clinical syndrome was described by investigators at Vanderbilt University Medical Center who reported on two cases of sudden and fatal myocarditis that occurred after combination immune checkpoint inhibitor (ICI) treatment. Since then, cases of ICI-induced myocarditis, while still rare, have been reported with increased frequency.
“We’re only seeing these rare side effects because immunotherapies are so successful and patients are surviving these deadly cancers,” said Javid Moslehi, M.D., director of the Cardio-Oncology Program at Vanderbilt.
The heterogeneous clinical presentation of ICI-associated myocarditis has made consistent identification of the syndrome a challenge. To facilitate identification and reporting, Moslehi and colleagues have proposed a formal definition of myocarditis.
“We built an international collaboration of experts in the field to define myocarditis.”
“Myocarditis can mimic a lot of other heart problems,” Moslehi said. “We built an international collaboration of experts in the field to define myocarditis – to outline how to describe the syndrome, and how to distinguish a case from someone suffering a heart attack, for example.”
Associated Cardiovascular Toxicities
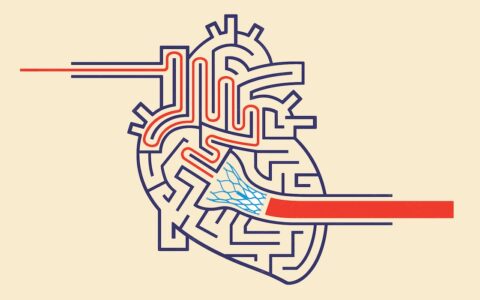
Myocarditis, or inflammation of the heart muscle, is one of several cardiovascular toxicities associated with ICIs, including vasculitis and pericarditis.
“Checkpoint inhibitors unleash the body’s own immune system to fight cancer. In the process of doing that, however, they can trigger your immune cells to become super active and interfere with the function of your heart and other organs,” Moslehi explained.
Adding to the complexity, ICIs are often combined with other therapies that can cause hypertension, arrhythmias, thrombotic complications, and vascular disease.
Systematic Characterization
The definition proposed by Moslehi and colleagues covers definite, probable, and possible myocarditis.
To monitor for the onset of myocarditis, the authors recommend that a baseline be established before beginning treatment against which changes can be evaluated. A baseline evaluation should include a physical examination, electrocardiography (ECG) and assessment of cardiac biomarker levels, specifically troponin.
The authors outline interval tests to evaluate subclinical myocardial injury as well as tests to be obtained if myocarditis is suspected. In general, patients who have a rise in cardiac troponin, ECG changes, arrhythmia or abnormalities of left ventricular systolic function should be considered for myocarditis and selected for adjudication.
Myocarditis often occurs quickly, Moslehi said, after just one or two doses of immunotherapy treatment. If myocarditis is detected, steroids can be used to dampen the immune response.
A Broader Understanding
Moslehi and colleagues hope a uniform case definition and systematic characterization of events will not only improve the ability of clinicians to capture this rare syndrome, but also facilitate documentation of the full spectrum of myocardial injury and permit consistent reporting across clinical trials.
“We hope this will enable a broader understanding of myocarditis and the range of clinical outcomes, and help identify high-risk groups,” Moslehi said.
“We hope this will enable a broader understanding of myocarditis and the range of clinical outcomes, and help identify high-risk groups.”