Ventricular shunts have historically been the standard treatment for newborns with hydrocephalus, but an endoscopic technique gives neurosurgeons a better option for a unique group of patients.
Researchers in a recent study demonstrated that endoscopic third ventriculostomy with choroid plexus cauterization (ETV/CPC) is even more effective for patients who underwent fetal repair of myelomeningocele (fMMR) than those who underwent myelomeningocele repair after birth. The study was conducted by the Neurosurgery Department at Vanderbilt University Medical Center.
Benefits of Prenatal Surgery
In myelomeningocele, the most severe form of spina bifida, the neural tube fails to close, exposing the open fetal neuropore to potentially caustic amniotic fluid. Traditionally, the myelomeningocele defect is closed after birth. While this minimizes the risk of meningitis, much of the harm to the nervous system has already taken place.
Pediatric neurosurgeon and principal investigator Michael C. Dewan, M.D., M.S.C.I., said prenatally repaired patients who are candidates for ETV/CPC may have better outcomes than those who have repair of their spinal defect after birth.
“We’re trying to minimize the morbidity, cost, and suffering associated with a lifelong VP shunt in fMMR patients by studying this more specialized treatment,” Dewan said. “We were very pleased to see that more than 90 percent of properly selected ETV/CPC patients can live a life shunt-free, granting patients and their families improved quality of life.”
The recent study explored whether prenatal surgery was associated with an improved response to ETV/CPC as measured by a reduced need for a shunt.
“From the 2011 MOMS study we know that the prenatally treated group is half as likely to develop hydrocephalus as is the postnatally treated group – about 40 percent versus 80 percent. ” Dewan said. “Now with the introduction of the ETV/CPC technique in the fetal myelomeningocele population, this study shows the proportion of patients that will ultimately require a shunt is further reduced by at least an additional 50%.”
Although the risk of hydrocephalus is significantly reduced, its occurrence still requires intervention. The traditional approach is to insert a ventricular shunt, a small tube placed in the ventricles and extending into the abdomen, to drain the excess cerebrospinal fluid.
Shunts vs. ETV/CPC
“When a child receives a shunt, it stays in their body for the rest of their life, leaving them at risk for blockage or infection which require emergent surgery to repair or replace,” Dewan said. “While some patients may go their entire lives without needing a revision, we’ve seen others who have required dozens of shunt revisions in their first 18 years of life.”
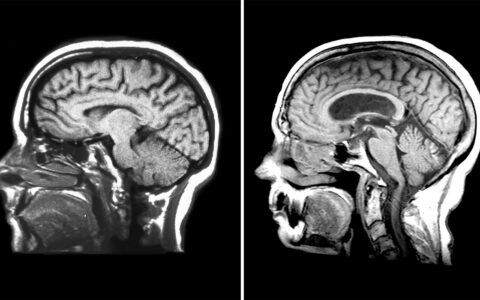
In the ETV/CPC procedure, the surgeon makes an incision in the infant’s scalp and inserts an endoscope into the brain ventricles. The ETV is then performed by making a small opening at the floor of the brain to allow the fluid an alternate drainage pathway, followed by cauterizing the choroid plexus to reduce cerebrospinal fluid production.
While a variety of anatomical considerations are important in deciding who should receive an ETV/CPC, the most important determining factor is the patient’s age.
“We know that very young patients do not benefit as much from ETV/CPC,” Dewan said. “For babies less than a couple months of age we often recommend a shunt as opposed to an ETV, because the likelihood of the ETV being successful is lower.”
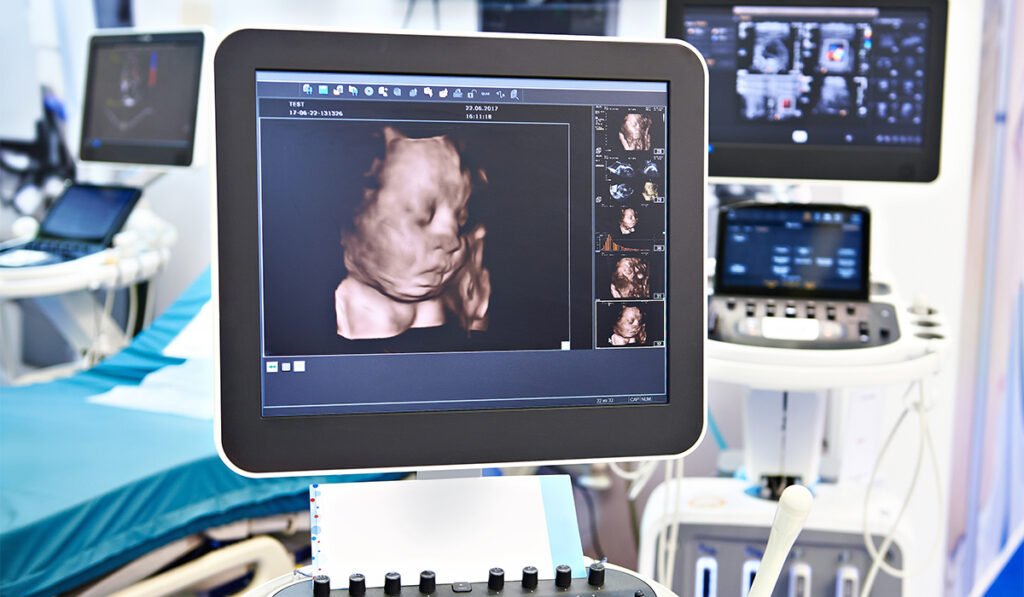
Fortunately, early after birth, hydrocephalus is rarely an emergent development. Because of this, neurosurgeons can regularly monitor the head circumference and obtain serial scans to see how the ventricular volume changes. With the opportunity to wait, the ETV/CPC option may become available as time progresses. Head or ventricle size enlargement or the development of other symptoms generally indicate that intervention is necessary.
Dewan’s team of researchers studied 88 patients who had undergone fMMR. Of those, 37 developed hydrocephalus; 16 underwent ETV/CPC while 21 received a shunt.
More than 70 percent of the children who received a shunt required at least one shunt revision operation. Meanwhile, only four of the 16 (25 percent) children who underwent ETV/CPC required any further surgery related to hydrocephalus. Among these four, three successfully underwent a “redo” ETV.
Cohorts Compared
While both interventions – fMMR and ETV/CPC – have by now been well-described, this study is the first to view them both in tandem. The evidence from Vanderbilt suggests there is a synergistic relationship between the procedures, significantly reducing the needs for shunts.
“The outcomes were overwhelmingly positive ,” Dewan said. “Fifteen of the original 16 patients who underwent ETV/CPC remain shunt-free. On the other hand, patients who received a shunt expended more healthcare resources (imaging studies and hospital readmissions) than their counterparts who underwent ETV/CPC.
Because this is the first study directly comparing ETV/CPC to VPS in an fMMR cohort, researchers are eager to test its reproducibility.
Affirmation Sought
“We want to join with other centers and get more numbers across a more diverse population and set of surgeons,” Dewan said. “So that’s exactly what we’re doing right now. Vanderbilt is a part of the 14-center Hydrocephalus Clinical Research Network, where we will be conducting a multicenter study in a similar fashion. By expanding the study population, we hope to further solidify the data demonstrated here at Vanderbilt.”