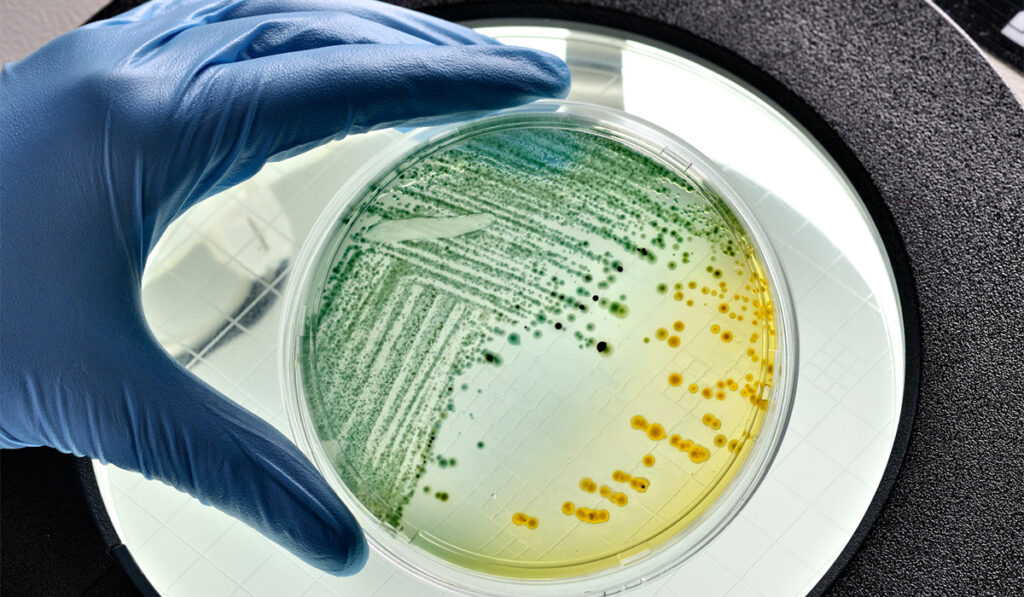
Researchers have discovered that certain commensal bacteria in the gut microbiota appear to provide protection against severe infections of pathogens such as Citrobacter rodentium and Escherichia coli.
Although the work by Vanderbilt University Medical Center has so far been done with mice, it raises the possibility of new treatments for diarrheal infections that cause more than 800,000 child deaths each year worldwide.
Bacteria affected are attaching and effacing strains that are characterized by lesions in the gut mucosa. There has been extensive research on these pathogens and the resulting immune response, but the role of the gut microbiota has not been as thoroughly examined. This study fills a part of that gap, according to Danyvid Olivares-Villagómez, Ph.D., an assistant professor of pathology, microbiology and immunology at Vanderbilt.
Olivares-Villagómez is co-author of the research study published in Infection and Immunity. He describes the results as “serendipity,” since the original research concerned granzyme B, a protease enzyme in killer immune cells.
Protective Cofactor Sought
Investigators observed that animals that were granzyme B-deficient had far more severe symptoms than other animals when infected with Citrobacter. Part of this difference was likely explained by the deficient T-cells themselves. However, in looking for a likely cofactor, researchers focused on the gut microbiota. The principal difference found was that the granzyme B-deficient animals had far less – and in many cases, none – of the commensal bacteria Turicibacter sanguinis.
These bacteria, whose mechanisms have not been widely studied, emerged as central to the research. Turicibacter is present in the microbiota of most vertebrates, including humans. Earlier studies of children with diarrheal infections showed that healthier patients have a higher level of Turicibacter than those who become sicker.
“This is significant for our research,” said Olivares-Villagómez. “That’s how we started working with Turicibacter.”
“The group of mice in the study which were initially deficient in the commensal developed protection when they were colonized with Turicibacter.”
Citrobacter is used to model E. coli in mouse studies because it does not require the use of antibiotics in test animals, as E. coli does.
“Treating the animals with antibiotics is cumbersome and also disrupts the microbiota, preventing us from observing the interaction between microbiota and host,” Olivares-Villagómez said.
Mice used in the study were initially deficient in the commensal bacteria but developed protection when they were colonized with Turicibacter. This is a good indication of causation, although the mechanism has not yet been defined, the investigator said. Ongoing follow-up research suggests that metabolites, as well as competition between organisms for specific niches, are likely mechanisms.
Olivares-Villagómez described a part of that research:
“We’re looking at metabolite composition in the intestine in animals deficient in Turicibacter and looking again after we colonize them with the commensal. We have detected some interesting metabolite hits, at least one of which appears to increase in vivo growth of the Citrobacter pathogen. When there is no Turicibacter, there is more of this metabolite. When Turicibacter is introduced, the metabolite decreases. Citrobacter ‘likes’ this metabolite, and the metabolite may make Citrobacter more pathogenic.”
Potential Therapeutic Paths for Diarrheal Infections
Although therapies for humans are not yet part of the picture, if the commensal is shown to provide protection from E. coli, Turicibacter and/or related metabolites could become part of a treatment.
“If the commensal is shown to provide protection from E. coli, then Turicibacter and/or related metabolites could eventually be part of a treatment.”
“Maybe Turicibacter provides a metabolite or depletes a metabolite,” said Olivares-Villagómez. “In that case, treatments could consist of increasing Turicibacter growth, for example with a probiotic pill, or giving patients a metabolite rather than the bacteria. Or, if the metabolite is harmful, preventing the metabolite from accumulating in the intestine. Such a treatment would be years away, but it is a possible path forward.”
Results of the research could apply to other commensal bacteria in the gut microbiota as well.
“There is a high probability that there are others,” Olivares-Villagómez said, noting the groundwork for additional investigation.