Families with children who have idiopathic scoliosis are often tempted to postpone corrective surgery until the patient’s late-adolescence or beyond, in place of an earlier intervention.
The impact of such deferrals on patient outcomes has been understudied, leading researchers at Vanderbilt University Medical Center to review 17 years of scoliosis surgeries, thereby isolating enough similar adult and adolescent cases to power an outcomes-comparison.
Byron Stephens, M.D., chief of the Division of Orthopaedic Spine Surgery, represented the Vanderbilt Spine Outcomes Lab as leader of the research in collaboration Scoliosis Research Society. This work was presented at the 2023 Pediatric Orthopaedic Society of North America.
“We wanted to know if there is a significant difference in outcomes between these two groups, and the short answer is: yes, there is,” he said.
“This crosses many measures, including the patient’s risk of complications, radiographic correction and need for revision surgery.”
“It’s generally better to proceed with the surgery in adolescence.”
The study looked at both clinical and radiographic outcomes. While the cohorts were small, the results can help guide clinicians in discussing surgical decisions with their patients and their families, Stephens said.
“These patients have the same surgical path, just at a different time. It appears, based on our dataset, that it’s generally better to proceed with the surgery in adolescence.”
Gray Area
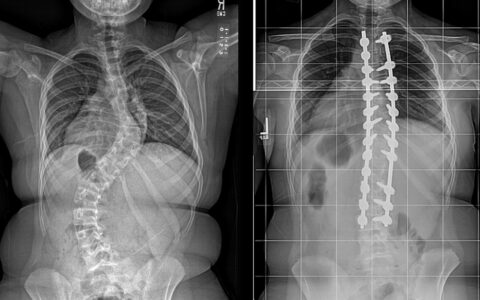
While the rarer infantile/early-onset scoliosis can threaten organ function, adolescent idiopathic scoliosis, which comprises the vast majority of pediatric scoliosis cases, is typically a skeletal problem with varying degrees of disfigurement and limitations in athletic abilities. For affected patients, the clinical approach toward mild to moderate curvatures is to observe or brace. In severe cases, the recommendation is spinal fusion at the curves.
When surgery is called for, the timing can be complicated by case-specific family factors and medical conditions, as well as varying views on best practices.
Two-to-One Comparison
To help clarify these issues, the Vanderbilt group matched 62 adult surgery patients two-to-one with 31 adolescent patients, all with similar pre-op curve characteristics. The mean ages were 26 years for the adult group and 14 years for the adolescent group.
Clinical and radiographic records were compared at two-year follow-up appointments. In radiographic comparisons, adolescents presented with a 12 percent lower major Cobb angle than in the adults. The adults also retained less correction in the coronal plane. No difference was found in the sagittal plane measures.
“The coronal Cobb angle has long been regarded as the primary measure of successful surgical correction,” Stephens said.
The adolescent group had a shorter average operative time, less blood loss and about half the complication rate. None in the adolescent cohort required post-op ICU care, while three of the adults were transferred to the ICU. The average length of stay in the hospital after surgery was 4.6 days for the adults and 3.8 days for the adolescents. Readmission and re-operation rates were about twice as high for the adult cohort.
While rare and ultimately resolved, the adult complications included pseudarthrosis, implant failure, neurologic complications and re-operation.
Spine Elasticity a Major Factor
Stephens says the higher complication rates and worse outcomes in adult patients are primarily due to the greater stiffness of the curves, requiring more invasive techniques to treat the same vertebra. While outcomes were not stratified for age comparison within the groups, he would expect to find overall outcomes to decline only slightly until complete skeletal maturity at around 30, then gradually decrease through middle age, deteriorating precipitously from late-middle age on.
“But, as we found, even the difference at the age of 26 is significant,” he said.
Stephens hopes that larger, multicenter, prospective studies will follow to affirm or more finely delineate these age-related differences.
“The odds of a good outcome skew toward earlier surgery.”
“In this realm, shared decision-making with the patient and their family is a central part of what we do,” he said. “We have good outcomes with both with adults and children, but this study provides data showing the odds of a good outcome skew toward earlier surgery. We hope it gives the clinician, patient and family greater peace of mind with respect to making the decision.”