Kidney reabsorption of magnesium is vital for homeostasis, but serum magnesium tests are not sufficiently sensitive to identify body magnesium deficiencies that can be harmful when combined with certain risk factors.
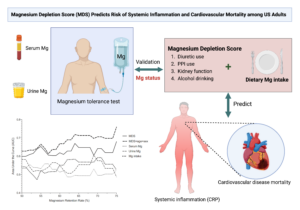
Nutritional epidemiologist Qi Dai, Ph.D., of Vanderbilt University Medical Center, has devoted his 30-year career to studying the interactions, impact and measurement of primary electrolytes and other nutrients in the body. He and Harvey Murff, M.D., director of the Division of Geriatric Medicine at Vanderbilt, Lei Fan, Ph.D., a Vanderbilt post-doctoral fellow, and other colleagues, developed a new tool, the magnesium depletion score (MDS), to more accurately determine magnesium deficiencies.
“Our models using the MDS, when combined with sex and age stratification, performed consistently better than other models in predicting magnesium status.”
“Serum magnesium testing, which is used clinically to diagnose deficiency, is tightly regulated, and therefore a poor measure of total body magnesium status,” Dai said. “Our models using the MDS, when combined with sex and age stratification, performed consistently better than other models in predicting magnesium status, and that predictive power may strengthen with the severity of the deficiency.”
Balancing Acts
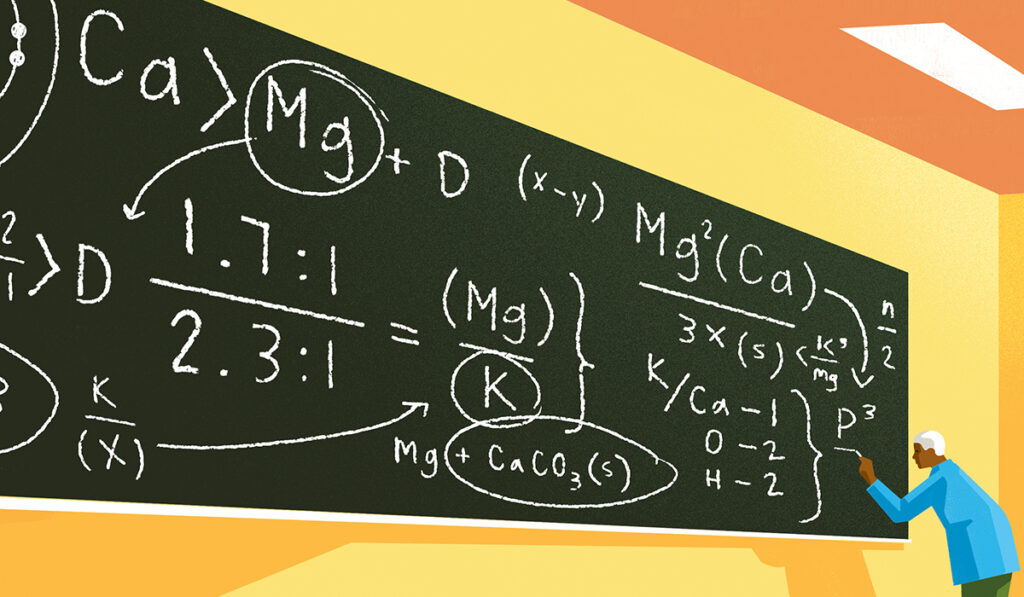
Dai’s work in recent years includes incursions into interactions between magnesium and calcium, and between calcium and vitamin D, and how the balance between them affects health. One randomized trial demonstrated the dependency vitamin D has on magnesium.
“We found an inverted U-shaped relationship between the two. If baseline vitamin D levels are low, magnesium supplementation will raise them, but if vitamin D levels are high, magnesium will lower them,” Dai said.
Similarly, the team has shown that a suboptimal ratio between magnesium and calcium is associated with colorectal adenoma and colorectal cancer, cognitive deficits, dementia, and other health risks.
Magnesium Depletion Score
Through these studies, researchers have identified a target range of 1.7:1 to 2.6:1 magnesium to calcium ratio, with 2.3:1 as ideal. Below this range, risks of cardiovascular disease mortality, cancer mortality, and incidence of dementia rose. Above it, high calcium intake may be detrimental and vitamin D status may be not optimal.
Knowing the importance of this ratio, Dai and his team then worked to develop a more effective way to estimate magnesium in the body. Serum and urine tests are not highly predictive, and the magnesium tolerance test (MTT), which is the gold standard, is overly labor-intensive, he says.
“The purpose of developing the MDS was see if our models could do better than existing clinical methods to make these measurements,” Dai said.
The MDS was tested in 77 patients who had combinations of risk factors of diagnosed chronic kidney disease, use of diuretics, use of proton-pump inhibitors or heavy alcohol use – all shown to reduce magnesium reabsorption. The researchers used the MTT for validation.
The team found a significantly higher area under the curve (AUC) for the MDS model alone (0.60) than for those using serum (0.53) or urine (0.58) magnesium measurements. Further, in the model that used MDS along with age, sex and intakes of magnesium and calcium, the AUC rose to 0.64 and may strengthen with the severity of the deficiency.
“This sample size is not sufficiently powered to infer conclusive estimations,” Dai said. “However, this is one of the largest and first studies comparing all these used methods against the MTT gold standard, and the results merit larger studies.”
Associations with Cardiovascular Disease
The team also risk-stratified the MDS and tested it for associations with inflammation levels and risk of cardiovascular disease mortality in over 10,000 United States adults from the National Health and Nutrition Examination Survey.
“Levels of inflammation significantly increased with increasing MDS scores, primarily among individuals with magnesium intake less than the estimated average requirement,” Dai said.
Getting the Ratios Right
Dai’s work underscores how correct measurement and attention to ratios matter in diagnosing, tracking and treating many inflammatory diseases.
“This lays a foundation for precision-based nutritional interventions.”
“The MDS serves as a promising measure in identifying who may benefit from increased intake of magnesium to reduce risks of systemic inflammation and cardiovascular disease mortality,” Dai said. “This lays a foundation for precision-based nutritional interventions.”