Recent increases in cancer survivorship are leading to populations of patients at risk of other lifelong conditions, including lymphedema, a blockage of the lymphatic system. Common cancer treatments including lymph node removal, radiation or certain chemotherapies can lead to lymphedema even years later in survivors’ lives.
“For breast cancer survivors, approximately 30 to 40 percent will develop lymphedema,” said Paula Donahue, D.P.T. , assistant professor of physical medicine and rehabilitation at Vanderbilt University Medical Center. “This is an enormous prevalence, yet we lack good prognostic indicators to determine the true at-risk populations. With improved indicators, we could tailor prophylactic therapies, treat high-risk patients sooner and reduce condition severity.”
Adapting MRI to Visualize Patient Risk
“MRI methods can be re-parameterized to visualize lymphatic flow dysfunction and associated tissue physiology changes relatively quickly and without injections.”
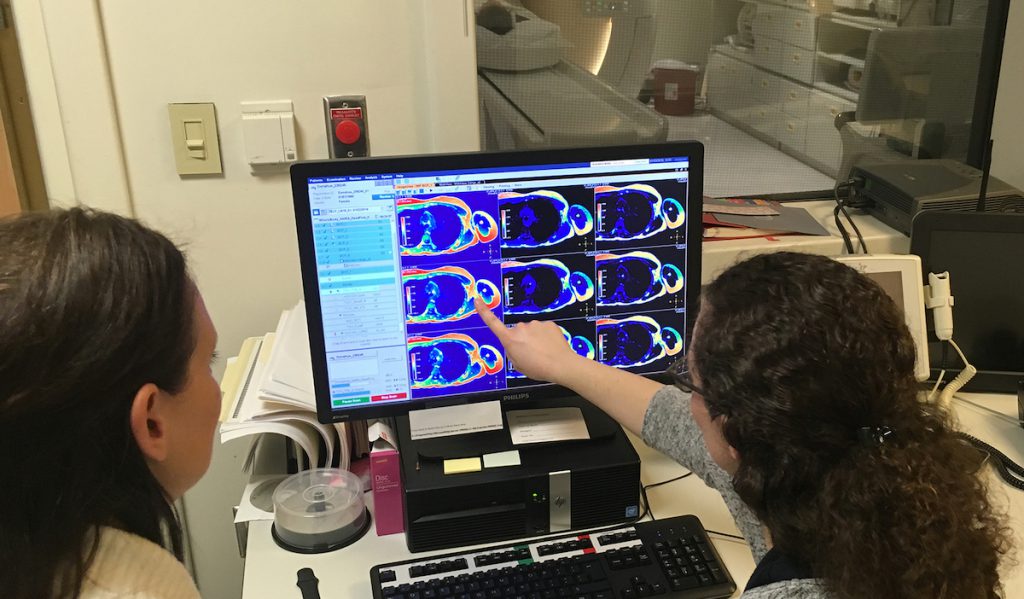
To better focus therapies, Donahue has partnered with radiology researchers at Vanderbilt to apply MRI techniques normally reserved for evaluating other circulatory conditions.
“The lymphatic system is central to maintaining fluid homeostasis and operates in coordination with the blood circulation,” said collaborator Manus Donahue, Ph.D., associate professor of radiology at Vanderbilt. “Our group is showing that MRI methods can be re-parameterized to visualize lymphatic flow dysfunction and associated tissue physiology changes relatively quickly and without injections.”
The group is using MRI for various aspects of treatment, including to map cancerous lymph nodes prior to surgery, to identify sub-clinical changes in lymphatic dysfunction post-surgery, and to quantify lymphedema therapy impact in symptomatic patients. They have begun their second NIH-funded clinical trial in this area.
“You wouldn’t angioplasty or stent a blood vessel without an angiogram,” Manus Donahue said. “Similarly, it’s nearly impossible to optimize lymphatic therapies without visualizing lymphatic circulation. Our initiative is to develop non-invasive tools customized for surveillance and evaluation of surgical, pharmacological and physical therapy-based interventions.”
Validating Treatment Approaches
The group has published a series of reports demonstrating translational applications of MRI for mapping lymphatics. Working with Rachelle Crescenzi, Ph.D., research instructor in the Vanderbilt University Institute of Imaging Science, the team quantified MRI relaxation times in lymph nodes, specifically healthy lymph nodes compared to those found in breast cancer patients.
“If we can quickly identify lymph nodes that are non-cancerous, we will know not to remove those nodes during surgery. This will reduce lymphatic disruption and lower a patient’s risk of developing lymphedema,” Manus Donahue said.
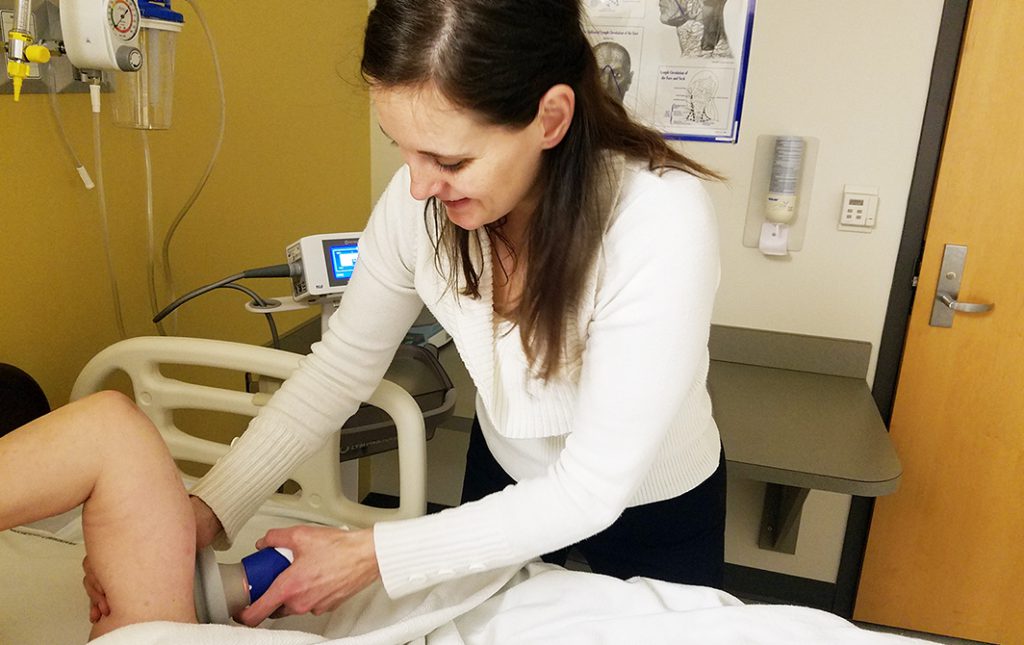
The researchers are also using MRI to validate therapy interventions. They have shown that the therapeutic technique of manual lymphatic drainage causes significant, beneficial changes to the deep tissue microenvironment. Such immediate changes, while detectable by MRI, are not possible to ascertain using common, less-specific bedside measurements.
Bringing Innovation to Physical Therapy
By performing MRI before and after physical therapy, the group can test new rehabilitation techniques for reducing lymphedema.
By performing MRI before and after physical therapy, the group can test new rehabilitation techniques for reducing lymphedema. They are now studying ways to enhance a commonly used approach, complex decongestive therapy (CDT).
CDT uses massage, compression, skin hygiene and targeted exercises to decongest lymph stasis, rerouting fluid to areas where it can be reabsorbed. The group is evaluating whether adding a graded negative pressure device to CDT can reduce excessive build-up of interstitial fluid, a major lymphedema contributor. MRI will not only help determine the device’s utility, but also whether certain patients have vascular profiles that predispose them to better outcomes.
“Based on the imaging, I can actually identify a patient’s intact lymphatic vasculature to better target clearance of their lymph congestion,” Paula Donahue said. “It’s a tremendous step toward more personalized medicine, especially when a person is less responsive to other management techniques.”