Collaborative care and innovative clinical trials have made Vanderbilt University Medical Center a nexus for treating brain cancer patients.
Ryan Merrell, MD, division chief neuro-oncology, and Alexander C. Mohler MD, associate professor, are two of the very few neuro-oncologists in Tennessee. They are part of a team of VUMC neuro-oncologists, neurosurgeons, radiation oncologists and medical oncologists who meet weekly to discuss specific patients and complicated cases. “We tend to see more patients than others because of our massive referral network,” Merrell said.
Tightening the Margins of Treatment
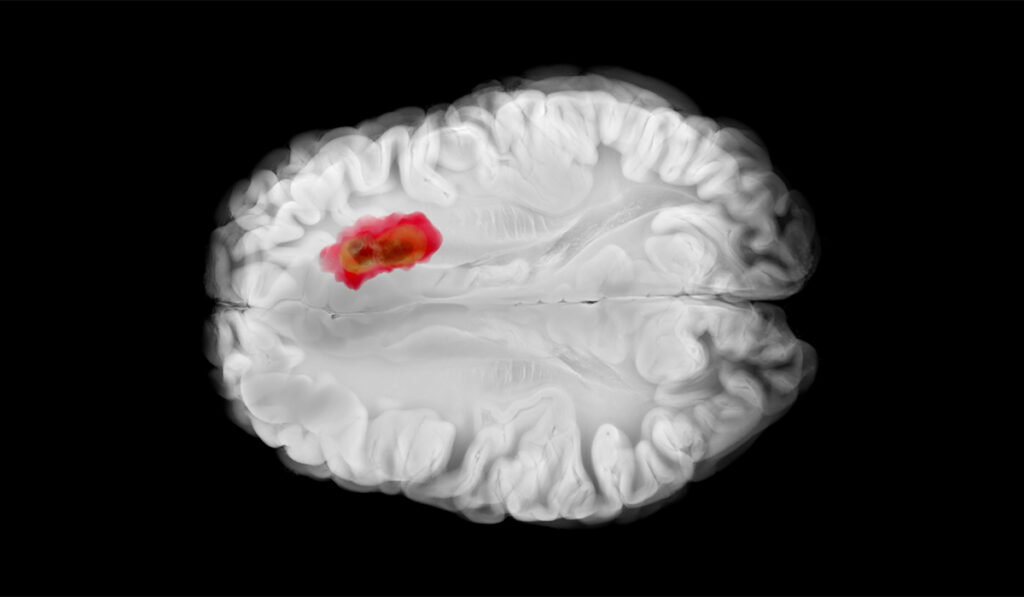
Brain surgery to remove metastatic tumors often leaves microscopic disease in the margins. Traditional external beam radiation, also called stereotactic radiosurgery, and follow-up radiation therapy four to six weeks later, leads to a local recurrence rate of 10% or higher.
Brachytherapy may offer a better option. Brachytherapy is common practice in prostate and genitourinary cancers, and has been used in brain cancers with radioactive iodine. Brachytherapy places radiation elements, such as seeds, into tissues to deliver a high dose of radiation directly at cancer cells. This minimizes radiation scatter and the amount of tissue irradiated by SRS, where radiation passes through other tissues to get to the target.
Researchers have continued to look for different delivery methods and isotopes for the brain. A new product, called GammaTile, provides surgically targeted radiation therapy immediately upon the completion of brain surgery. Small, soft tiles use Cesium-131 as a radiation source to penetrate 5 millimeters into the tumor cavity in the brain and yield a tight margin of radiation just around the tumor or alongside it. This provides equivalent local recurrence-free survival to stereotactic radiotherapy.
“GammaTile has the advantage of immediate radiation effect, with no need for follow-up appointments for radiation treatment,” said Lola B. Chambless, MD, professor of neurological surgery and radiation oncology. “Our neuropathologists can read a frozen specimen of brain tissue within 20 minutes to ensure that the diagnosis is accurate, which allows the surgeon to place GammaTile. Many other centers send out specimens, which takes a week or more, and means that intraoperative use of GammaTile is not an option.”
Chambless is a principal investigator in the Post-Surgical Stereotactic Radiotherapy Versus GammaTile-ROADS (Radiation One and Done Study, or ROADS). This Phase 3 randomized controlled trial will compare the efficacy and safety of intraoperative radiation therapy using GammaTile versus SRT following tumor resection of newly diagnosed metastatic brain tumors. The head-to-head trial in about 80 centers nationwide plans to enroll several hundred patients.
The ROADS trial will examine neurocognitive outcome. VUMC is the only facility in Tennessee participating in the trial. Ten patients have enrolled, and enrollment will continue for a few more months, with results expected within six months.
Multiple Applications for GammaTile
GammaTile can also be applied to different brain tumors, from primary glioblastomas to aggressive meningiomas. VUMC is participating in several GammaTile brain cancer clinical trials, looking at both efficacy and the potential to reduce serious complications, such as radiation necrosis. Conventional SRT leads to a 20% incidence of radiation necrosis, with tissue damage from radiation appearing months to years after treatment. “The death of tumor cells creates a cascade of edema in the brain. This creates a dilemma for the neuro-oncology team – is this edema or the tumor recurring?” Merrell said.
Less Invasive Approaches
Another clinical trial for brain metastasis patients, run by VUMC’s Anthony J. Cmelak, MD, director of head and neck radiotherapy and director of functional radiosurgery, will test the efficacy, radiation necrosis and neurocognitive effects of three radiation fractions versus the traditional one fraction. If successful, “this will open the door to treating more lesions with radiation alone without surgery,” Merrell said.
“We minimize exposure to normal tissue and provide post-op pain control to allow the patient to recover as soon as possible.”
The multicenter trial has enrolled 20 patients at VUMC, with enrollment open for another year.
The goal of brain cancer treatment is to reduce morbidity and induce quick recovery. “We minimize exposure to normal tissue and provide post-op pain control to allow the patient to recover as soon as possible,” Chambless said.