Hydrocephalus and other disorders of the cerebrospinal fluid (CSF) typically require lifelong monitoring of cranial pressure and brain structure changes, as well as potential symptoms such as headaches.
Whether the disorder developed in infancy or later from injury or disease, many young patients get lost in the transition from pediatric to adult care or, alternatively, in a chain of referrals that ultimately ends without a defined care plan.
In 2024, Reid C. Thompson, M.D., chair of the Department of Neurological Surgery, along with Kelly M. Brown, M.D., director of the Neuroscience Patient Care Center at Vanderbilt University Medical Center, were inspired to create a multidisciplinary medical home for such patients. The result was the new Hydrocephalus, Chiari, and CSF Disorders Center serving patients from throughout the mid-South and Southeast.
Next, they recruited Ryan Lee, M.D., a neurosurgeon from the CSF Disorders Center at Johns Hopkins Hospital, where he trained and performed research.
“Much of my role is to serve as a champion for these patients, many of whom have had multiple complex surgeries, so they get coordinated and specialized care,” Lee said. “Historically, patients with these multifaceted medical issues can end up getting bounced around and no one is looking at the big picture.”
The Center’s Design
Besides hydrocephalus, the center also serves patients with Chiari malformations, pseudotumor cerebri (idiopathic intracranial hypertension), CSF leaks, syringomyelia, tethered spinal cord, and cysts of the brain and spine.
This breadth of care requires not just neurosurgeons, but an array of other specialists, including neurologists, radiologists, ophthalmologists, physical therapists, and neuro-interventionalists, brought together for a combined effort to provide individualized care and collaborate on research.
“Historically, patients with these multifaceted medical issues can end up getting bounced around and no one is looking at the big picture.”
“Since opening in October 2024, we’re seeing about 50 patients a week in clinic and already doing 10 to 15 related surgeries and procedures per week.”
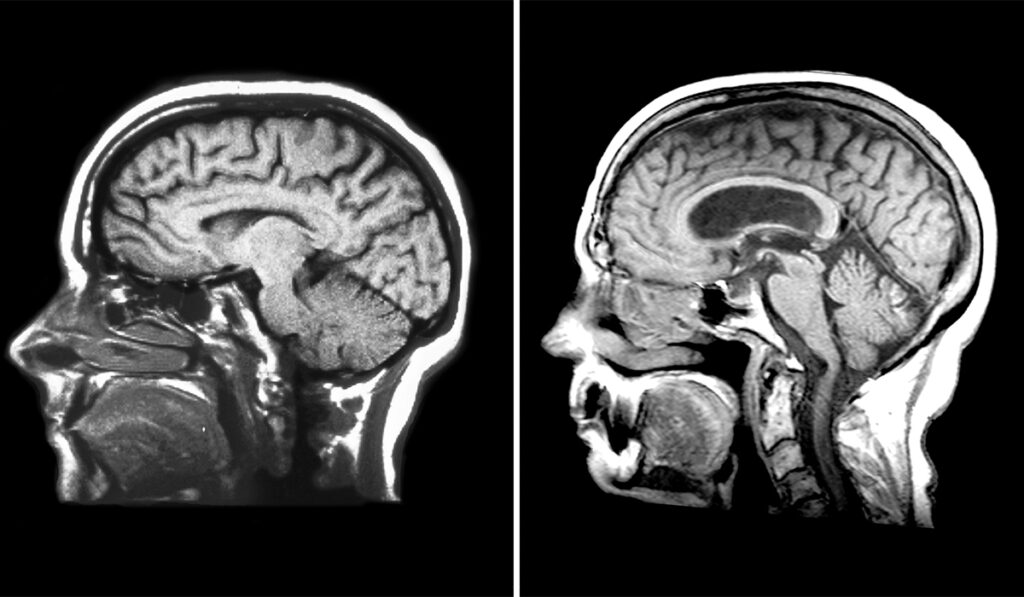
The research component will focus on analyzing clinical outcomes data, improving diagnostic tests, and collaborating with engineers to create innovative ways to image the brain without the radiation of CT scans or the cost and burden of MRI scans.
Widening the Net
Lee says that while many pediatric neurosurgeons have expertise in hydrocephalus and other CSF disorders, very few adult neurosurgeons are equipped to treat complex patients. Yet, patients with hydrocephalus constitute a large proportion of neurosurgery patients, including those needing initial treatment and the majority who require lifelong monitoring and care.
Lee says they will focus on stemming the loss of transitional patients in the 18- to 20-year age range, who typically have graduated from a well-resourced pediatric care experience and fail to acquire regular adult care. Younger adults often fail to get regular imaging and follow-up until the patient requires a trip to the emergency room.
The center is also escalating screening for Normal Pressure Hydrocephalus (NPH).
“Only about 20 percent of NPH patients are receiving treatment,” Lee said.
Some lack a proper diagnosis, as the condition can be overlooked due to symptoms that mimic the side effects of aging, including balance problems, dementia and incontinence.
“With this new center, we are at minimum doubling our capacity for doing these screens and shortening the wait for the patient,” Lee said. “This is the only reversible cause of dementia, and we should never miss a chance to turn someone’s life around.”
Window into the Brain
Vanderbilt will also be offering the ClearFit implant made of a sonolucent (ultrasound penetrable) material known as polymethyl methacrylate that enables ultrasound imaging of the brain.
This technique allows ultrasound to replace many of the CT and MRI scans now used for monitoring the brain, particularly in hydrocephalus and Chiari malformations, and at a lower cost and with lower exposure to radiation and contrast agents.
Lee has used this implant material to cover burr-holes as small as two centimeters in diameter instead of using bone graft or allowing natural closure. He was first author on a study of sonolucent burr hole covers that laid the groundwork for its effective and safe use.
“While the resolution is not as high as in CT or MRI, advances have enabled a very adequate visualization of the ventricles, so we can assess changes in CSF volume,” Lee said.
Plus, the implant enables a patient who experiences bad headaches, for example, to avoid an ED visit or a long wait for a CT scan by having an in-clinic assessment.
Lee has been teaching this technique around the country, most recently at a national course in Colorado. He will soon publish a paper on measurement applications for a new imaging technique.
“Neurosurgeons are coming to learn this technique, and it’s really exploding across the country,” he said. “We are excited about offering it as one of the centerpieces of our new center.”