Patients with acute heart failure may be at increased risk of kidney injury, but how that happens in the body has been unclear. A new study finds extracellular vesicles (EVs) – vesicles that circulate in the bloodstream – may play a role in this process.
EVs carry vital molecules throughout the body in health and disease and are gaining traction as key mediators of disease response. While some are protective, such as in the case of exercise-induced EVs, others can increase disease risk.
Ravi Shah, M.D., director of clinical and translational research in the Division of Cardiovascular Medicine and an adult heart failure cardiologist at Vanderbilt University Medical Center, co-led the study, published in JCI Insight, with his long-time collaborator at Massachusetts General Hospital, senior author Saumya Das, M.D., Ph.D.
The researchers employed studies in patients with heart failure and an organ-on-a-chip model of the human kidney to show how EVs contribute to kidney injury. They describe biologically relevant pathways that circulating EVs may impact within kidney cells during heart failure, including those that contribute to kidney disease.
Extracellular Transport
Shah explains that vesicles are constantly “budding off” from different cells, circulating as tiny cargo ships transporting an array of molecular mediators, including metabolites, proteins, lipids, transcripts, non-coding RNA, and more.
“EVs can provide a means by which molecular information traffics across different organs,” Shah said.
EVs and their cargo loads have diverse functions, including stimulating biologic responses, sending signals across the body’s organs, and fueling cancer growth. Das and Shah’s team used liquid biopsies to study EV contents and identify specific molecules that could serve as biomarkers for cardiovascular disease.
“We want to know how vesicles are altered in cardiovascular disease states and whether they contain transcripts relevant to disease progression,” Shah said.
Kidney-on-a-Chip
Inflammatory EVs are known to surge during heart failure, but Das and Shah’s team is the first to connect them to cardiorenal syndrome, a commonly occurring comorbidity in patients with heart failure who are exposed to large amounts of diuretics acute illness.
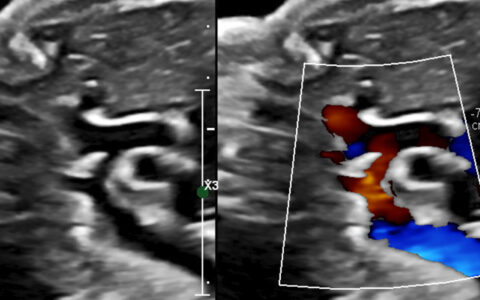
The researchers used an organ-on-a-chip model to recapitulate what happens at the blood-kidney interface. The innovative system employs human-derived cells to build small pieces of a specific organ, like renal epithelium.
The main benefit of organ-on-a-chip models is that researchers can use this microfluidic technology to expose the chips to different biofluids, Shah explained.
“You can actually use humanized cells and completely parse the effects of some exposure in that tissue alone.”
EVs Damage Renal Cells
The researchers exposed their kidney-on-a-chip models to circulating EVs from patients who had experienced acute heart failure. Some of the patients also had renal dysfunction – or cardiorenal syndrome.
EVs from patients with cardiorenal syndrome were found to activate known markers of renal injury in the cells on the chip model. The researchers describe gene regulatory transcripts, including microRNAs, inside these EVs as the drivers of injury.
“Pathways that we saw as perturbed in the chip may actually replicate disease in humans,” Shah said. “This is striking to me, because it provides two-level validation. Not only is the chip a reasonable model, but it also suggests that what we’re finding may be translatable.”
“Pathways that we saw as perturbed in the chip may actually replicate disease in humans.”
Therapeutic Applications
Shah imagines EVs as a potential drug target, given the availability of RNA-based therapeutics.
“You could target RNA inside EVs to restore kidney function or prevent its decline, not only in cardiorenal syndrome but potentially in hemodynamic states like acute kidney injury, post-cardiopulmonary bypass, or others.”
The researchers are now testing whether depleting – or increasing – certain EV transcripts has any beneficial effect in their kidney-on-a-chip model. There’s lots more to come, Shah says.
“We focused on transcripts, but there’s a lot of other things within those vesicles: lipid metabolites, proteins, and longer transcripts. It’s quite possible given the complexity of all the biology that a lot of this working in concert. We just dissected one part of it.”