Pro-inflammatory agents that emerge following lung injury have a beneficial effect on healing, yet overproduction of these agents also may inhibit normal lung repair.
Seeking to differentiate between the types of macrophages and their effects, investigators at Vanderbilt University Medical Center conducted a mouse-model study using groundbreaking techniques to determine which kinds of macrophages play what roles in lung repair.
“Our work may enable us to track these different macrophages and understand their differing biology – something people have been really confused about for a long time,” said principal investigator Timothy S. Blackwell, M.D., director of the Division of Allergy, Pulmonary and Critical Care Medicine and the Center for Lung Research. “Ultimately, we want to see if these mouse-model findings are reproducible in humans and learn if different subtypes quell inflammation and promote normal versus fibrotic repair.”
The research by Blackwell and first author Wei Han, M.D., of the Division of Allergy, Pulmonary and Critical Care Medicine at Vanderbilt, was published in the Journal of Immunology. It is expected to pave the way for better identification of specific targets that could improve outcomes from inflammatory conditions, including pneumonia.
Search for ‘the Bad Guys’
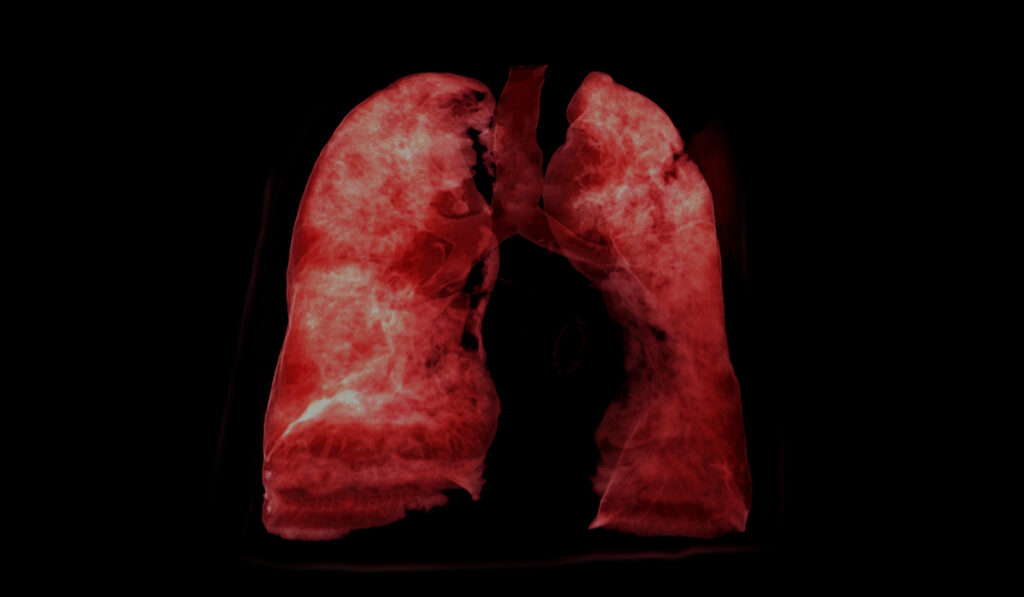
Macrophages, including the tissue-resident type and those recruited from the blood, produce cytokines and mediators that ramp up inflammation to fight pathogens in the lung. Persistent activity after the crisis is averted can lead to lung injury and fibrotic remodeling, explained the researchers.
Three types of macrophages are present during the entire process: resident alveolar macrophages (AMs), bone marrow (BM)-derived macrophages, and interstitial macrophages.
“Identifying subtypes helps us figure out which are the good guys, and which are the bad guys that we want to target.”
“The question has been which macrophages – resident or recruited – are responsible for what roles and how could we manipulate their actions to drive a healthier process,” Blackwell said.
The investigators developed a technique to separately label AMs- and BM-derived macrophages with a fluorescent lipophilic dye, and then used fluorescence-activated cell sorting, FACS, to quantify them.
“Identifying subtypes helps us figure out which are the good guys, and which are the bad guys that we want to target,” Blackwell said.
Missing Alveolar Macrophages
The pursuit of a differentiator began when Han was using a rodent model to investigate how aging affects inflammatory responses in the lung.
“Older people have a much higher mortality rate from conditions like acute lung injury and pneumonia than younger people,” Blackwell said. “That’s thought to be because they have a dysregulated inflammatory response.”
Hence, he and Han were looking for mechanisms that led to persistent inflammatory responses in old mice compared to young mice. When using standard flow cytometry developed for identifying subsets of macrophages and other inflammatory cells, they found that alveolar macrophages seemed to largely disappear.
“Were they dying and getting replaced by new ones, or were they ‘hiding’ into the tissue?” Blackwell asked.
They couldn’t find evidence that they were dying, and lymph node dissections did not show that they were leaving the airway, leading the researchers to wonder if the cells were just changing their surface markers in dynamic ways.
Digging deeper, they placed a membrane-bound fluorescent dye into the airway to label resident alveolar macrophages. This confirmed that these cells, indeed, changed their surface markers.
Acute Lung Challenge
Next, they hoped to clearly differentiate AMs from macrophages coming from the circulation (BM-derived). Han successfully injected the fluorescent dye into the bone marrow of a mouse’s tiny tibia, and after instillation of bacterial lipopolysaccharide, was able to see the bone marrow cells start to move to the lung.
“Using dyes with different colors to separate the two types of cells, we were able to sort out macrophages based on where they came from at multiple time points after the inflammatory stimulus, and then look to see how they changed both in terms of number and characteristics,” Blackwell said.
Toward Modifying Disease
The researchers also found that BM-derived macrophages were enriched in expression of genes involved with signal transduction pathways and immune system activation, whereas resident AMs were enriched in cellular processes, such as lysosomal and phagosomal pathways, efferocytosis, and metabolic pathways.
“Our ultimate goal is to use technologies like this, along with things like single-cell sequencing, to help us identify subsets of cells that are over-represented in aging mice, and possibly aging humans, and that contribute to disease,” Blackwell said.
“These could be specifically targeted by medications or biologics to reduce their number or change their phenotypes to ones that are reparative.”