Emerging reports have raised awareness of a hypercoagulable state associated with COVID-19 that causes an increased risk of thrombosis.
Now, a new case series suggests that this risk may extend to the eye, highlighting an association between COVID-19 and the development of retinal vein occlusions in otherwise young, healthy patients.
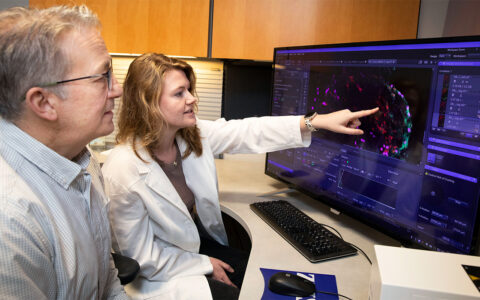
Led by ophthalmologist Avni Finn, M.D., of Vanderbilt University Medical Center, the series describes 12 cases of retinal vein occlusion in patients ages 18 to 50 following a COVID-19 diagnosis.
The good news: all but one patient had partial or complete resolution of their ocular symptoms.
“The majority of patients at their final follow-up had good vision and maintained good vision,” Finn said, “and very few required treatment with anti-VEGF injections, which many patients who are older and have retinal vein occlusions complicated by macular edema or neovascularization require long-term.
“Patients with visual changes who have either a recent COVID-19 diagnosis or active COVID-19 illness and are symptomatic with certain visual changes should be seen by an ophthalmologist and evaluated for retinal vascular disease.”
Following the Thread
Finn initiated the study after a patient in his 30s with COVID-19 was referred to her for new visual symptoms. She diagnosed the patient as having a central retinal vein occlusion and, knowing the link between COVID-19 and coagulation dysfunction, reached out to colleagues to inquire whether they had seen similar cases, which they had.
Retinal vein occlusions in young adults are quite rare, Finn explains, usually occurring in people over 50. Leading risk factors include diabetes, hypertension, cardiovascular abnormalities, and glaucoma.
“The majority of patients at their final follow-up had good vision and maintained good vision, and very few required treatment with anti-VEGF injections.”
“That was really the impetus for putting together a case series of patients in a younger age group,” Finn said. “We wanted to see what risk factors these otherwise healthy patients had, how they are doing, and whether there is a potential association with COVID.”
A Clean Cohort
For the study, Finn solicited cases through various societies and networks for retina and macula specialists. Only those cases that matched strict inclusion criteria – such as an absence of diabetes, hypertension, cardiovascular disease, glaucoma, obesity, and pre-existing thrombophilia – were included.
“By excluding things that we know put patients at risk for retinal vein occlusions, we could then more cleanly say these cases are potentially associated with the COVID-19 rather than other risk factors,” Finn said.
Of the 12 patients included, 75 percent were diagnosed with central retinal vein occlusions and 25 percent with hemi-retinal vein occlusions. The median time from COVID-19 diagnosis to ocular symptoms was just under seven weeks, with a median of 10.5 days of reported symptoms before ophthalmic diagnosis.
At follow up, the vast majority of patients had achieved visual acuity of 20/40 or better; however, four patients showed retinal thinning on imaging by the end of the study interval. In addition, five patients presented with macular edema, which was either observed for resolution or treated with anti-VEGF injections.
Counseling Providers and Patients
Finn notes that patients do not have to be critically ill with COVID-19 to exhibit retinal manifestations. Only three patients in the case series were hospitalized for management of COVID-19, and none were intubated.
When physicians suspect that a patient with COVID-19 and ocular symptoms has retinal vascular changes, she recommends an evaluation of their levels of D-dimer and fibrinogen, two markers of inappropriate blood clotting that have been reported abnormal in patients with COVID-19.
“There have been some studies of patients with COVID-19 showing that those levels remain elevated for months after infection, so they may be at greater risk for arterial or venous events after their illness,” Finn said.
“The biggest takeaway is that these were all young patients, and they all did quite well and had almost complete resolution of the event, which is valuable information when counseling patients with vision changes.”