Wilms tumor is the most common renal malignancy of childhood, making up approximately 90 percent of all pediatric renal tumors, and are typically addressed by upfront, primary resection, followed by adjuvant therapy based on tumor stage and biology.
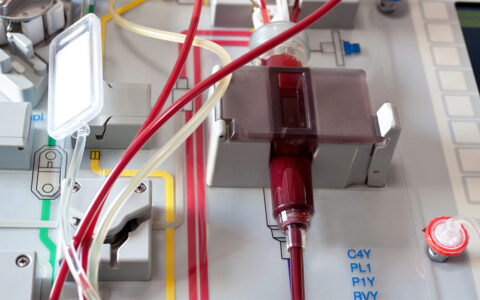
Harold “Bo” Lovvorn III, M.D., and Daniel Benedetti, M.D., of the Children’s Oncology Group at Monroe Carell Jr. Children’s Hospital at Vanderbilt, have recently introduced minimally invasive surgery (MIS) via laparoscopy as an option for patients who receive chemotherapy before resection, or about 20 percent of Wilms tumor cases.
The physicians, who conduct research on and provide care to children with intra-abdominal malignancies, have a special interest in the treatment of Wilms tumor. They point out that the less-invasive technique has several potential benefits for children with intra-cavitary solid tumors. These benefits include smaller incisions, shorter length of stay and reduced postoperative pain.
Lovvorn and Benedetti hypothesized that this technique, in the context of neoadjuvant chemotherapy, could be a better option for resecting Wilms tumor in children and helping keep patients on time for their next treatment, whether that’s additional chemotherapy or radiation.
“Over the past two decades, we’ve been asking the question: How can we be less invasive, cause less pain and keep our children on time for their next therapy cycle?” Lovvorn said. “We first published on MIS in Wilms tumor in 2010, and we’ve continued to build upon these results since.”
Growing Experience
In considering MIS for the surgical management of Wilms tumor, the researchers first characterized optimal candidates for MIS resection following neoadjuvant chemotherapy. Then, they assessed the impact of the operative approach on maintenance of therapeutic schedules.
After their retrospective analysis, the researchers found that MIS resection of neoadjuvant-treated Wilms tumor in appropriately selected patients achieves equal oncologic fidelity and better maintains post-surgery treatment plans.
“Oncologic fidelity was equal across surgical approaches to Wilms tumor after neoadjuvant chemotherapy, as no significant differences were found in margin status, tumor spill, sampling or involvement of lymph nodes, or relapse-free and overall survival,” Lovvorn said.
Another novel observation was that the MIS resection significantly reduced time to resume chemotherapy for patients relative to open operations, the researchers found.
Furthermore, in appropriately selected patients, MIS resection of Wilms tumor appeared to reduce opioid consumption and to promote earlier discharge, which are important considerations in pediatric cancer care.
“Early resumption of multimodal therapy is important to mitigate disease progression after tumor resection, especially if preoperative rupture or spread to lymph nodes had occurred,” Lovvorn said. “And MIS is one possible avenue for maintaining children on strict therapy schedules without additional delays,”
This approach and treatment strategy also is of critical import to children with genetic syndromes that predispose them to development of Wilms tumor and have the need to preserve as much kidney function as possible to avoid future dialysis, Lovvorn explained.
Questions Remain
The researchers said the reason for longer delays in open procedures remains unclear, but it is potentially related to the extended convalescent times needed for open procedures, the need for longer durations on opioid pain medication, delays in time to ambulation, and nuances in oncologic care.
Lovvorn and Benedetti both acknowledged the study had limitations. Notably, the sample size was small, and the retrospective nature of the study limited data collection and further generalization of the findings. Nevertheless, it provides important information in the absence of a true randomized study for MIS compared with open resection of Wilms tumor or any pediatric embryonal tumor.
Concluding Remarks
Differences in surgical expertise with MIS techniques for embryonal tumor resection likely exist, and MIS approaches may not be broadly used or accepted by some pediatric surgeons, Lovvorn said. Nevertheless, he and Benedetti hope that these results will help increase awareness and support for this technique within the pediatric oncology surgical community.