Blood clot avoidance is an under-met need for women taking chemotherapy for ovarian and other gynecologic cancers.
In 2019, the American Society of Clinical Oncology (ASCO) issued guidelines for venous thromboembolism (VTE) chemoprophylaxis that provided evidence for preventative measures for patients with cancer. In an effort to improve adherence, gynecologic oncologist Alaina J. Brown, M.D., and her team at Vanderbilt University Medical Center conducted a quality improvement initiative to alert providers regarding chemotherapy patients at high risk for VTE.
“Since this is a relatively new ASCO guideline, busy clinicians may not be used to calculating these scores along with all the other preparations they make for a patient’s chemotherapy,” Brown said. “We hoped to assist in notifying clinicians if a patient was a potential candidate to start VTE chemoprophylaxis with their chemotherapy.”
Brown and her team used risk-score assessments to identify patients who were of moderate to high risk for blood clots, and then set up provider alerts linked to the higher-risk patients. After this change, 50 percent more clinicians ordered prophylactic blood thinners for their patients.
More Options for Prevention
About 100,000 Americans die each year from VTE. About half of all blood-clotting events occur in the three months following surgery or a hospital stay, and approximately one in 10 hospital deaths are associated with pulmonary embolism.
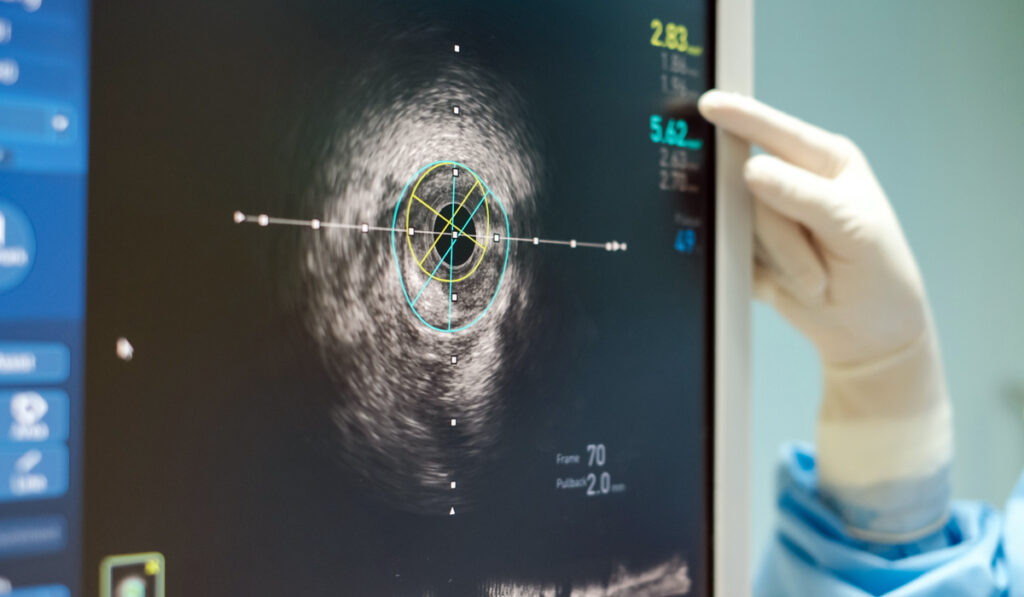
While most patients today are up and walking soon after surgery, more can be done to lower the risk of VTE, according to the Agency for Healthcare Research and Quality, which cites an “implementation gap” in VTE prophylaxis between best practice and real-world practice. The agency also calls for “evidence-based protocols that standardize VTE risk assessment and prophylaxis.” These would include more routine measures, like pressure-cuffing and mobilizing patients, as well as ultrasound surveillance, to help guide medically complicated decisions on prophylactic blood thinners.
Gynecologic Cancers Examined
While most VTE development occurs in the hospital, outpatients who are undergoing chemotherapy for gynecologic cancers also need preventative efforts. A study of 112 patients with ovarian cancer who did not receive prophylactic therapy found that 11 percent developed a VTE during neoadjuvant chemotherapy, 6 percent post-operatively, and another 10 percent during adjuvant chemotherapy.
“We are hoping our work contributes to greater awareness of who is at risk and will ultimately improve and broaden VTE prevention.”
Brown says good risk-assessment tools are available, including the Khorana score for patients with solid tumors and lymphomas. Levels of risk between zero and six are assigned based on type of cancer, pre-chemotherapy platelet count, hemoglobin level or red blood cell growth factors, leukocyte count and BMI.
Getting a Heads-up
To first establish baseline risk, Brown and her team retrospectively reviewed the charts of 62 patients with gynecologic cancer and calculated the Khorana scores. Half of the Khorana scores were at or above level two, the ASCO threshold for considering blood thinners in the absence of contraindications.
None of the 62 patients had received VTE chemoprophylaxis, and seven (11 percent) developed VTE. All seven had Khorana scores of three or four. Although a score of two is the ASCO threshold for starting VTE chemoprophylaxis, this level confers no greater risk, while the VTE risk was 15 times higher in patients with a score of three or higher.
The team executed their quality improvement initiative by adding an alert that flagged patients’ Khorana scores for clinicians to view prior to ordering chemotherapy. They then examined a post-intervention cohort of 22 and found that 11 had received chemoprophylaxis, per the guidelines. None of the 11 patients developed VTE or experienced other adverse effects related to VTE chemoprophylaxis.
Opportunities and Landmines
Brown and her team are currently evaluating other ways to decrease cancer patients’ risk of developing VTE.
“We’re also working on a mechanism for calculating CAPRINI scores, a post-surgical assessment of VTE risk, for minimally invasive surgical patients to ensure that all patients are leaving the hospital on the proper VTE prophylactic medication, if indicated,” she said.
“The guidelines on this are evolving. We want to personalize VTE risk stratification so that our patients’ individual level of VTE risk may be considered in all our protocols.”
The debate over the best blood thinners for cancer patients is ongoing, with oral agents like apixaban gaining favor for patients at lower risk of major bleeding episodes.
“This is an area of medicine where balancing the risks and benefits of prophylactic medication may be tricky. We are hoping our work contributes to greater awareness of who is at risk and will ultimately improve and broaden VTE prevention,” Brown said.