An automated text messaging program delivering friendly reminders and health advice for patients with type 2 diabetes (T2D) sustained a high level of patient engagement over a 12-month period. It did so among diverse patients who have not typically been well represented in studies of this type.
The research, published in JMIR mHealth and uHealth, was conducted by a Vanderbilt University Medical Center team that included Lyndsay Nelson, Ph.D., a research assistant professor of medicine, and Lindsay Mayberry, Ph.D., an associate professor of medicine.
“Diabetes patients with low socioeconomic status, and patients from racial or ethnic minority groups, haven’t been well represented in the literature on mobile health interventions, even though they may be at highest risk for nonadherence and worse outcomes,” Mayberry said.
Mayberry and Nelson, who have collaborated previously to identify risk factors contributing to worse diabetes outcomes among Black, non-Hispanic Americans, are now focused on optimizing implementation of their mobile health (mHealth) program.
“There’s evidence that adding a human component to technology-delivered self-management programs is more effective than offering the technology program alone, especially among vulnerable groups,” Mayberry said, adding that this issue has never been studied directly or within an implementation framework.
Value of Continuous Texts
Most prior research into text messaging interventions for diabetes care has looked at patient engagement over a three-month or six-month time period. The Vanderbilt study was part of a larger randomized, controlled trial – REACH, for Rapid Education/Encouragement And Communications for Health – and expanded the analysis to a yearlong intervention that focused on enrolling diverse patients.
Study participants were literate, English-speaking patients with T2D from community health centers and Vanderbilt primary care clinics. Their average age was 56 and 41 percent had an annual household income below $25,000. All patients had been prescribed a daily diabetes medication, for which they were responsible, and owned a mobile phone with texting capabilities.
Participants received text messages that pertained to either medication adherence or to self-care behaviors such as eating healthfully. For the first six months, all participants received at least two texts daily. After six months, patients were given the choice to receive fewer texts or continue with daily texts.
Mayberry and Nelson found that the best text message content was affirming, positive and appropriate for all health literacy levels.
“In the trial, we found that 44 percent of participants, or nearly half, chose to stay with the daily texts at the six-month mark,” Nelson said. “I believe their choice to continue daily texts speaks to the quality of the texts.”
Engaging Patients in Content Creation
Engaging the patients themselves in the content of the texts proved instrumental to the efforts’ success. “We designed the intervention with and for these patients,” she said.
For example, during usability testing, patients pushed back on messages that began: “If you missed your medicine today…” or “If you fell off your routine…”
“Patients responded, ‘Don’t presume we’re not doing what we’re supposed to do,’” Mayberry said.
“In the trial, we found that 44 percent of participants, or nearly half, chose to stay with the daily texts at the six-month mark.”
Reducing Barriers to Adherence
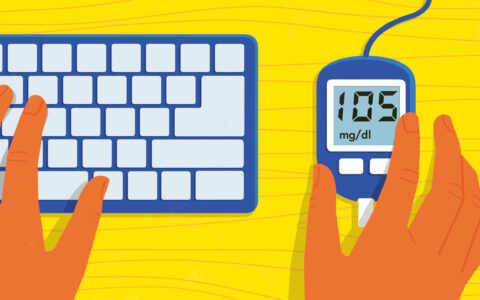
While the program significantly improved medication adherence and dietary behavior up to 12 months, “treatment effects were not significant for any outcome at 15 months,” the authors wrote in a paper published in Diabetes Care reporting on REACH’s outcomes. They concluded that “REACH reduced barriers to adherence, but barrier reduction did not mediate outcome improvements.”
Additional components such as counseling with a pharmacist, diabetes education, or health coaching may help to address some of the barriers to medication adherence, such as beliefs or behavioral skills deficits, the researchers said.
Mayberry and Nelson also interviewed participants who received the intervention and clinic staff to understand REACH’s implementation potential. They expect to publish these results within the next three months.
Comparing Approaches for Implementation
In a grant application recently submitted to the Patient-Centered Outcomes Research Institute, Mayberry and Nelson propose to find the best way to implement mHealth programs like REACH in community health centers.
“We designed the intervention with and for these patients.”
Their goal is to compare offering mHealth two ways. One way will be as a supplement to clinical care, with patients using mHealth to monitor and support their own self-management. The other approach involves integrating mHealth into care in a way that enables clinicians to view patients’ data from mHealth and use it to inform office visits and between-visit treatment.
The researchers want to see whether integrating mHealth with clinical care has benefit for patients beyond supplementation. “Offering it as a supplement requires fewer clinic resources but viewing and acting upon the patient-generated data it collects may lead to larger effects on patient outcomes,” Nelson said.