Untreated hearing losses have known associations with depression and cognitive function. Individuals with impaired hearing are often cut off from multiple sources of social support, information and stimulation. Yet despite the availability of treatment to restore near-normal auditory comprehension, only five percent of candidates for cochlear implant receive it.
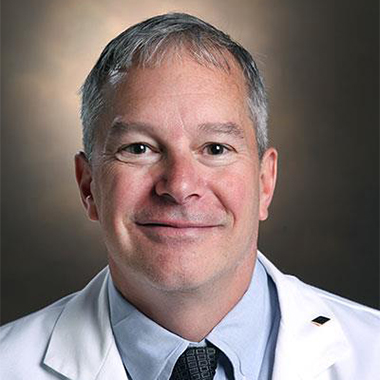
“As a field, we feel somewhat embarrassed by the fact that 95 percent of adults who stand to gain from them are still not getting this help,” said David Haynes, M.D., chief of the Neurotology Division at Vanderbilt University Medical Center.
Haynes says the reasons are multifaceted, but all addressable. He leads Vanderbilt’s cochlear implant clinic – one of the largest in the world. There, his team is tackling the major deterrents to making the procedure a better-understood, better-publicized option, with a low burden of visits and financial uncertainty. “Several years ago, we started a process to identify and break down barriers, and we mapped out the entire process that is now coming into full fruition with our new cochlear implant bundles,” he said.
In 2020, Haynes was the primary investigator on a paper in JAMA Otolaryngology-Head and Neck Surgery establishing consensus guidelines to formalize cochlear implants as standard of care for patients with moderate, sloping to profound, sensorineural hearing loss.
Barriers to Assent
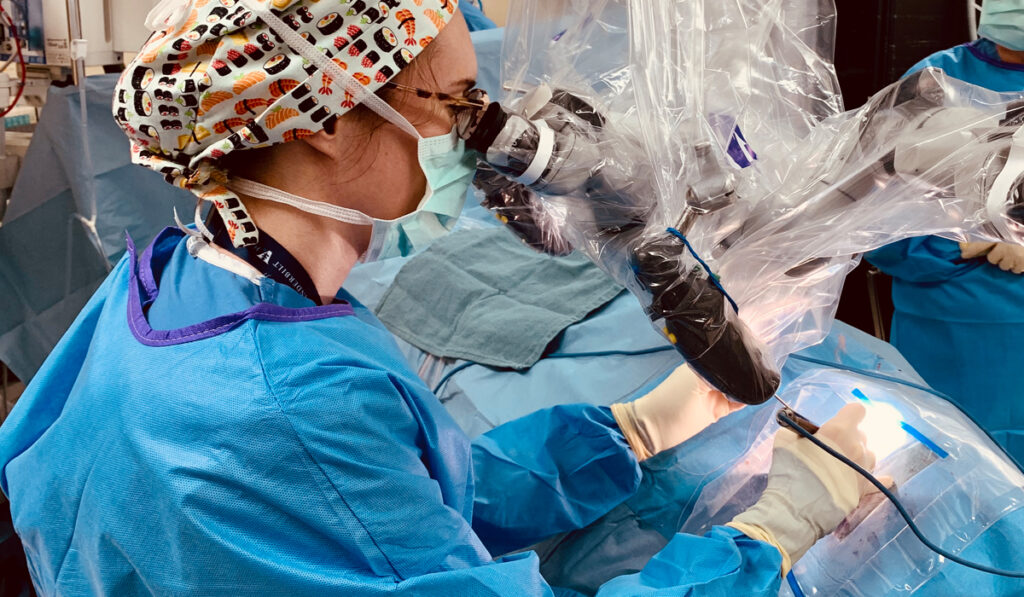
Haynes says the decision to get an implant is not an easy one, but today’s device advancements are lowering the barriers. The implant surgical procedures are shorter, the internal device is smaller, and the external devices have a lower profile. Most important, the cochlear electrode array that makes distinctions in sound waves and the external speech processors have improved tremendously in the past few years.
One of the deterrents for patients, he says, is the complexity of making multiple trips for audiology testing, imaging, pre-op testing, surgery and then programming of the device. Said Haynes, “Some of our patients were driving 250 miles or more back and forth, up to ten times.”
Vanderbilt is addressing this by offering single-day services. “The patient comes in in the morning for hearing tests, anesthesia evaluations, radiology and surgical consults,” he said. “Our anesthesia and surgical teams are prepared to perform surgery that afternoon, if that path is chosen.”
At the Vanderbilt clinic, programming is often done the day after surgery. Subsequent fine-tuning can be accomplished in person or remotely through telehealth.
Another barrier has been the complex array of billing processes and financial question marks that traditionally accompanied such a procedure. Vanderbilt is tackling this through MyHearingHealth, the first bundled cochlear implant program in the world.