The REACH for Survivorship Program (REACH) offered by the Vanderbilt-Ingram Cancer Center is expanding its umbrella of care through new services, including heightened follow-up care for prostate cancer patients and a grant-based program to extend telehealth and patient navigator services to remote rural areas.
“We want to bring our programs into the community as opposed to having the community come to our campus,” said REACH director Debra Friedman, M.D., E. Bronson Ingram Chair and director of pediatric hematology-oncology at Vanderbilt University Medical Center. “Our goal is to bring survivorship services to the people who need them most.”
“We want to bring our programs into the community as opposed to having the community come to our campus.”
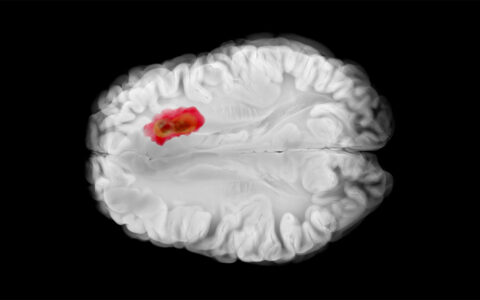
The U.S. population of cancer survivors is quickly increasing and by 2029 will include 29 percent of the population or about 22 million people. National guidelines recommend survivorship care that includes disease surveillance and health promotion to reduce chronic health issues and the risk of cancer recurrence.
Reaching a Reluctant Group
REACH is working with Vanderbilt’s urology department to arrange for prostate cancer patients to receive survivorship care sooner after surgery than they had been receiving such services. Men who had undergone prostate cancer surgery at Vanderbilt often neglected advice from their nurse practitioner or urologist to contact the survivorship clinic. A surprising number were simply tolerating serious post-surgical complications, including genitourinary functional incontinence, which clearly warranted discussion with a clinician.
“Often they were just living with these problems, instead of seeking help,” said Friedman.
To address these issues, Elizabeth Winkler, the nurse practitioner with REACH, has collaborated with the urology team to generate personalized patient reports on outcomes measures. Patients and their clinicians receive specific information about the kinds of symptoms the patient can expect to experience, how long to expect those symptoms to last, and how to proceed if symptoms persist. Winkler now schedules patients for their post-surgical visits.
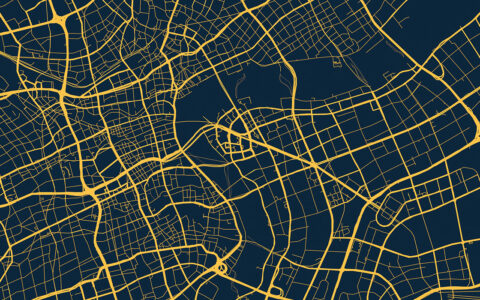
Services Sans Travel
Friedman received a grant from the National Cancer Institute to learn more about the needs of cancer survivors who live in underserved, rural communities and to institute a program to better serve these areas. “Some of these patients live two or three hours away from the hospitals where they had received treatment,” said Friedman.
Telehealth and patient navigator services will be provided under the grant. The clinic also will be hiring and training two local patient navigators and training nurses at sites within the Vanderbilt Health Affiliated Network serving Tennessee and nearby states.
The concept is that patient navigators who live in and know rural locales can steer patients to resources close to their homes. Patients can find local services for health maintenance.
Telehealth services provided in rural areas are covered by the Center for Medicare and Medicaid Services, as well as by commercial insurers.
Improving Access for Other Patients
The REACH clinic sits on the main campus of Vanderbilt University Medical Center while the Vanderbilt Breast Center is located about five miles to the southeast at the One Hundred Oaks campus. Winkler will now spend one day each week at the breast center, which Friedman says will make a big impact by not requiring a special trip when patients are under so much stress.
“Breast cancer patients have been going for their surgical or medical follow up appointments to the breast cancer clinic and did not want to make a second trip to the REACH clinic. We learned that this was a barrier that kept patients from coming in for survivorship services,” said Friedman.