A majority of patients with multiple sclerosis (MS) who are experiencing the facial pain of trigeminal neuralgia (TN) stand to benefit from consideration for microvascular decompression surgery (MVD), according to a recent study published in World Neurosurgery. The findings provide clarity about the controversial treatment option, which some surgeons do not offer to MS patients with TN due to the wide variation in reported rates of pain freedom.
“Although MVD has proven to be a very effective approach to treating trigeminal neuralgia, when it comes to using the procedure in MS patients, there’s been a fair degree of debate and disagreement,” said lead author Danika Paulo, M.D., a resident in neurological surgery at Vanderbilt University Medical Center.
The researchers analyzed the degree of success achieved using MVD to treat TN facial pain in MS patients, as well as the demographic and preoperative factors that might be associated with successful use.
Targeting Pain’s Root Cause
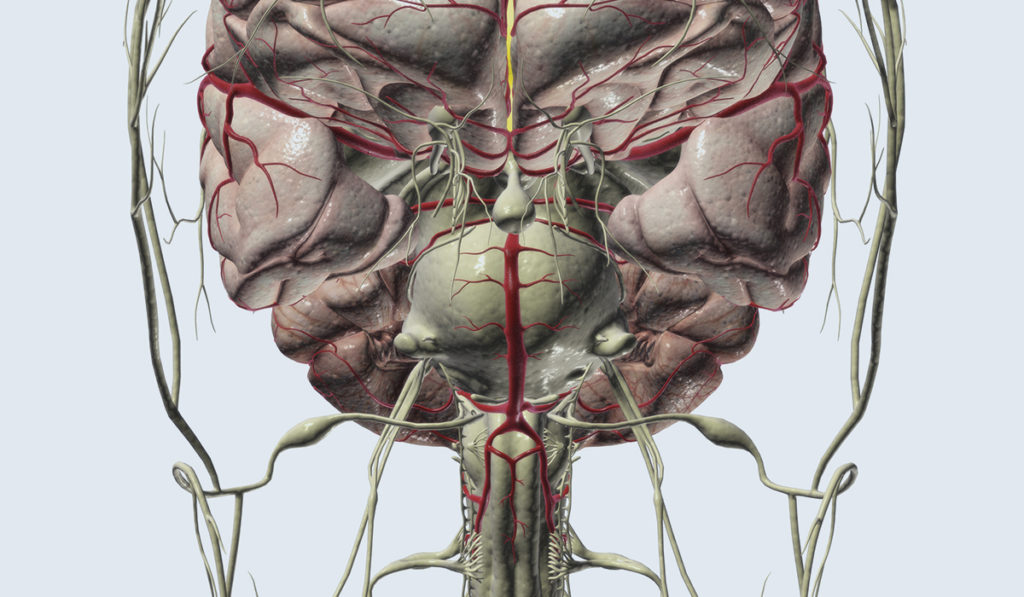
The usual cause of TN is a blood vessel pressing upon the trigeminal nerve at the base of the brain, causing that nerve to malfunction. Various facial stimuli – from drinking a hot or cold beverage, to a light touch or breeze, to just smiling – can trigger TN pain. Patients often describe TN as feeling like a jolt or electric shock, and the pain can lead to uncontrollable episodes of facial twitching. TN facial pain can increase in intensity and duration from mild to excruciating, to the point that it is debilitating.
MVD is unique among medical and surgical treatments for TN in that it eliminates the anatomical compression causing the pain. The surgeon enters through a small incision behind the ear and drills into the skull to access the brainstem and visualize the blood vessel or other abnormality impinging upon the nerve. MVD is the most common surgical procedure used to address TN pain, with a high overall success rate.
Treating TN in MS Patients
Paulo and colleagues performed a retrospective analysis of 33 patients who had been diagnosed with MS and who were experiencing TN. The patients had all been treated for their facial pain with MVD at Vanderbilt between 1997 and 2017.
The researchers assessed preoperative data that included demographic variables such as age, sex, and weight. They also included details of each patient’s MS and TN history, such as the severity of the TN pain, as ranked on the Barrow Neurological Institute (BNI) pain severity scale.
The study found that at a mean follow up time of about 4.5 years, 22 of the MS patients (67 percent) were still experiencing a significant reduction in their TN pain. MS patients whose BNI pain severity scores were relatively high before MVD were more likely to have unfavorable outcomes after the operation than patients with less severe preoperative pain.
Focusing on Patients with Less Severe Pain
Patients’ preoperative pain scores proved to be the only factor that was significantly associated with the success of the surgery. Sex, MS subtype, and the presence of MS plaques were among the other factors not significantly associated with the success of MVD.
“Our findings suggest that clinicians need to select MS patients who are suitable for MVD carefully,” Paulo said. Specifically, clinicians should keep in mind that the patients with the most severe facial pain phenotypes proved less likely to benefit from MVD, but that pain relief can still be achieved for carefully selected patients in this unique population.
“Our findings suggest that clinicians need to select MS patients who are suitable for MVD carefully.”