Patients on maintenance hemodialysis (MHD) bear increased risk for novel coronavirus disease COVID-19 and its complications, making it “crucial to rapidly deploy appropriate preventive strategies in outpatient hemodialysis facilities,” said Alp Ikizler, M.D., of Vanderbilt University Medical Center in a new editorial in American Journal of Kidney Diseases.
“Patients on maintenance dialysis are likely to be at increased risk of COVID-19 and its complications because they tend to be of older age and to have multiple co-morbid conditions such as hypertension and suppressed immune systems. The logistical aspects of MHD such as recurrent physical presence at health care facilities and physical proximity of patients during hemodialysis further increase the risk of disease transmission,” said Ikizler, who is Catherine McLaughlin Hakim Chair in Vascular Biology and director of the Vanderbilt Division of Nephrology.
“The logistical aspects of MHD such as recurrent physical presence at health care facilities and physical proximity of patients during hemodialysis increase the risk of disease transmission.”
Current Knowledge
Ikizler notes that it is not yet possible to accurately describe the incidence of COVID-19 in MHD patients, nor is it possible to provide detailed information regarding the clinical course of the disease in MHD patients. Much of the existing MHD data are from the epicenter of the disease in Wuhan, China, or from other areas with high infection rates and are not yet peer-reviewed.
“There are some scattered reports from the Northwest Kidney Centers and others that suggest that a handful of people who have become COVID-19 positive are on MHD,” Ikizler said, “but there are no reports of any widespread transmission among MHD patients.”
Strategies for Reducing Risk
Nephrology teams should follow guidelines from the Centers for Disease Control and Prevention (CDC), which can also be accessed at the American Society of Nephrology website. In addition, several dialysis organizations have developed their own guidance documents, Ikizler said. These documents are considered “interim” and are expected to evolve as more information is gathered.
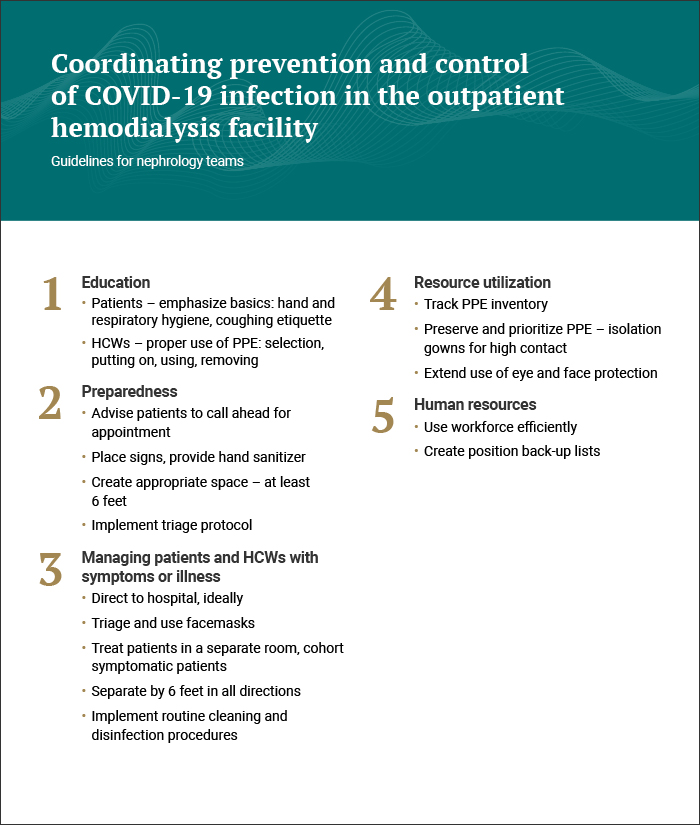
The documents contain detailed instructions on how to coordinate efforts in outpatient hemodialysis facilities. Ikizler broadly categorizes these efforts into: education, preparedness, managing symptoms or illness, and resource utilization.
Education
Patients and health care workers in dialysis units should be educated about COVID-19 on an ongoing basis. Details regarding hand and respiratory hygiene, as well as cough etiquette, should be emphasized regularly. Clinicians should be educated about the selection and use of personal protective equipment (PPE), including practicing how to put on, use and remove PPE.
Preparedness
Prepare the dialysis unit waiting area with appropriate signage, provide hand sanitizers and allow space of at least six feet between individuals. These efforts should be accompanied by a triaging plan to identify patients with fever or symptoms of respiratory infections before they enter the treatment area. Instruct patients to call ahead to report fever or respiratory symptoms.
Managing Symptoms or Illness
Currently, patients with symptoms should be directed to hospitals rather than be dialyzed in isolation in hemodialysis facilities – unless the facility can fully comply with the CDC’s guidance. However, if inpatient hemodialysis units reach capacity, patients with symptoms or mild illness will have to be dialyzed at outpatient facilities.
Ikizler says if this is the case, symptomatic patients should ideally be dialyzed in a separate room with the door closed. If a separate room is not available, treatment should be performed at a corner or end-of-row station, and the symptomatic patient should be masked and separated by at least six feet in all directions. He notes CDC guidance does not require that COVID-19-infected patients be treated in an airborne infection isolation room.
Dialysis facility hepatitis B isolation rooms may be repurposed for COVID-19-infected patients only if the facility has no hemodialysis patients with hepatitis B infection who require treatment in these rooms. Multiple patients with symptoms or illness may be placed together at a specific section of the unit and during the same hemodialysis shift, preferably the last shift of the day.
Resource Utilization
In addition to keeping track of PPE inventory, additional efforts should be employed for preserving PPE. These include prioritizing isolation gowns for procedures that generate aerosolized body fluids and for high-contact patient care activities, as well as implementing extended use of eye and face protection.
Efficient workforce utilization along with appropriate planning for peak disease activity is crucial. “Each unit should create a back-up list for all positions that could be utilized in the event of a possible increase in disease activity or a decrease in workforce due to illness,” Ikizler said.
Future Implications
Academic centers and large dialysis organizations should rapidly create data collection tools that can complement the basic clinical data collected by CDC and state health departments, Ikizler said. “Only then will we have reliable information to get ourselves prepared for the next inevitable epidemic.”
“Only [by collecting data] will we have reliable information to get ourselves prepared for the next inevitable epidemic.”





