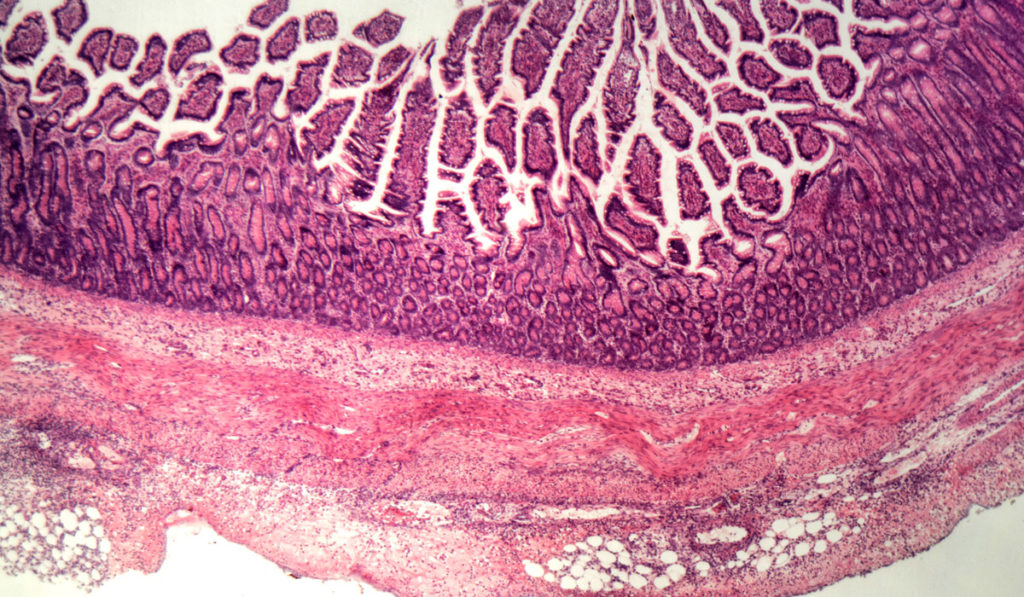
Therapy with tumor necrosis factor (TNF)-alpha inhibitors has been life altering for the 1.3 million people in the U.S. with inflammatory bowel disease bowel disease (IBD). However, because of the immunosuppressive characteristics of TNF-alpha inhibitors, long-term use has been noted to increase the risk of serious fungal infections like Histoplasma capsulatum (histoplasmosis), with rates of infection three times more frequent in patients taking TNF-alpha inhibitors than tuberculosis.
A new case series, published in Inflammatory Bowel Diseases by investigators at Vanderbilt University Medical Center, has shown that there may be other biologics that are as effective and have a lower risk for fungal infection. Prior series of histoplasmosis infections associated with TNF-alpha inhibitors have included a combination of IBD and non-IBD diagnoses and have not described IBD-related outcomes.
“We wanted to be able to prescribe an alternative therapy with confidence.”
“We practice in an area where histoplasmosis is endemic, so we’ve experienced patients who have had this infection,” said Sara Horst, M.D., associate professor of gastroenterology at Vanderbilt. “We wanted to be able to prescribe an alternative therapy with confidence.”
Study Results
Horst and colleagues conducted a retrospective chart review of patients treated at the Vanderbilt Inflammatory Bowel Disease Clinic between November 2011 and January 2018. Seventeen cases were identified with a diagnosis of disseminated or pulmonary histoplasmosis. All but one, who was on tofacitinib, were on a TNF-alpha inhibitor at the time of diagnosis.
Ten patients (58.8 percent) required re-initiation of biologic therapy at a mean of 383 days after initiation of histoplasmosis therapy. Seven patients were treated with the gut-specific agent vedolizumab, two with anti-TNF agents, and one with ustekinumab after diagnosis of histoplasmosis. Three patients with early recurrent IBD symptoms were given intravenous immunoglobulin (IVIG) before restarting a biologic agent.
At the end of follow-up, 15 of 17 individuals had maintained surgery-free clinical IBD remission without recurrence of histoplasmosis. Notably, this included patients with active disease at the time of infection, and only one ulcerative colitis patient in the series required surgery for refractory disease activity.
“We maintained very close infectious disease follow-up during therapy,” Horst said. “TNF is the natural inhibitor that kills histoplasmosis and we wanted to make sure we treated the infection. The anti-integrin compounds don’t target the TNF pathway as directly.”
Implications for Practice
Horst wants practitioners to be aware of the possibility of histoplasmosis, especially in areas such as the Southern U.S. where the infection is prevalent.
“We do a urine test or chest X-ray before we start people on anti-TNF therapy to look for fungal infection,” Horst said.
Patients on TNF-alpha inhibitors who have histoplasmosis typically present with very high fever and cough which is non-responsive to antibiotics and sometimes accompanied by diarrhea or mouth ulcers. “The most important thing is for us to counsel our patients,” Horst said. “Explain what the risks are; let your patients know when to call you.”
“Before four years ago, it was really difficult to take someone off anti-TNF… Now, we have new biologics that are a great alternative.”
Horst believes biologics such as vedolizumab represent a viable alternative to TNF-alpha inhibitors—especially since TNF-alpha inhibitor re-initiation was avoided in all but two patients in the study. “Before four years ago, it was really difficult to take someone off anti-TNF—it was the only thing that helped them. Now, we have new biologics that are a great alternative.”