The landmark, seven-year National Institutes of Health-funded trial, Management of Myelomeningocele Study (MOMS), established clear benefits for babies who underwent open fetal neurosurgery for myelomeningocele, the most severe form of spina bifida. The procedure, in utero repair of myelomeningocele, was pioneered at Vanderbilt University Medical Center in 1997, and Vanderbilt was one of only three participating centers in the MOMS study.
In the MOMS data, prenatal repair of myelomeningocele was shown to significantly decrease the risk of death or the need for shunting. As compared with postnatal surgery, it improved scores for mental and motor function, and the likelihood of a child being able to walk unassisted. The study proved that some factors causing Chiari II malformation and hydrocephalus can be reversed if the myelomeningocele is repaired before 26 weeks of gestation. However, the study did show an association between early intervention and increased risk of maternal and fetal complications.
“This was the first well-controlled study demonstrating the benefits of fetal surgery for this condition,” said Ronald Alvarez, M.D., chair and clinical service chief of Obstetrics and Gynecology at Vanderbilt. “It showed the real potential to meaningfully affect physical function in a child affected by spinal defects.”
Improving Outcomes in Fetal Surgery
Today, The Fetal Center at Vanderbilt, part of Monroe Carell Jr. Children’s Hospital at Vanderbilt, is continuing to fine-tune the prenatal myelomeningocele procedure.
“Vanderbilt has built considerable expertise in fetal surgery,” said J. Michael Newton, M.D., Ph.D., assistant professor of Obstetrics and Gynecology. “We’ve been doing the spina bifida surgery from the very beginning and have performed over 270 procedures. Through the years, we have continued to modify the procedure so that our outcomes are some of the best in the country.”
Open fetal surgery is performed by a dedicated team: two maternal-fetal medicine specialists, a pediatric neurosurgeon, a pediatric plastic surgeon, a pediatric cardiologist, a dedicated obstetrics anesthesiologist, and a dedicated OR team. The team is led by Kelly Bennett, M.D., professor of Obstetrics and Gynecology and director of Maternal Fetal Medicine. Bennett is an internationally recognized expert in the care of high-risk pregnant mothers and babies born with birth defects or anomalies.
“It’s not uncommon to have dedicated providers,” said Newton, “but at our center the surgery is performed by same team, every time, without variation. Careful, scripted post-op care is also a critical part of the protocol.”
A Coordinated-Care Approach for Fetal Anomalies
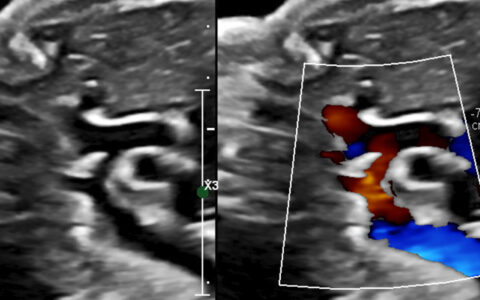
While myelomeningocele patients represent the majority of the fetal surgeries at Vanderbilt, the Maternal-Fetal Medicine team at the Fetal Center collaborates in the care of all mothers with ultrasound findings of fetal anomalies, plus women referred for high-risk maternal conditions.
“We like to see those mothers here because we can coordinate prenatal care with all the pediatric subspecialties and direct their care for optimum outcomes,” explained Newton. “Even if they’re not a candidate for fetal surgery, we still work with the referring obstetrician to monitor the mother during pregnancy, and most have their babies at Vanderbilt because of the strength of our NICU.”
The Future of Fetal Surgery
Advances in bioengineering and fetal surgical techniques are enabling the expansion of fetal therapies to address other conditions. These interventions, such as fetoscopic procedures, are improving outcomes already and will continue to do so in the future.
“This is a growing specialty for us,” said Alvarez. “We want to expand to other types of fetal surgeries for larger patient populations. We know the impact it can have benefitting newborn children.”