Despite many advancements through the years in scoliosis surgery, shoulder-height imbalance remains an undesirable result in up to a quarter of patients.
“The surgeon’s primary goal in posterior spinal fusion is to achieve the best spine alignment for each patient, but there hasn’t been much exploration into this secondary issue of post-operative shoulder imbalance,” said pediatric orthopaedic surgeon Craig R. Louer, M.D., at Monroe Carell Jr. Children’s Hospital at Vanderbilt. “Yet, its rates have been shown to be as high as 25 percent, with cosmetic deformity linked to lower patient satisfaction.”
Earlier studies have evaluated the relationship between the degree of primary thoracic curve and shoulder-balance outcomes, yet a treatment algorithm that consistently arrives at the correct shoulder alignment has remained elusive. After mulling over pertinent factors and reviewing the research, Louer decided to look more closely at two key measurements: 1) the degree of flexibility at a point proximal to the thoracic curve slated for correction, and 2) the degree of upper-instrumented vertebral tilt.
He then arranged for their mutual cancellation to be a goal in his surgeries, calling it the “flexibility-tilt agreement.” Finding success with this approach, Louer led a retrospective study of radiographs taken over 17 years. He and his team tested the multiple variables at play, eventually demonstrating that achieving flexibility-tilt agreement was the strongest predictor of post-operative shoulder balance, by far.
Factors in the Balancing Act
The study was focused, first, on learning how achieving agreement between flexibility and vertebral tilt, along with other perioperative variables, affects post-operative shoulder balance. Second, he examined deformity characteristics that may occur when this agreement is achieved.
The researcher defined flexibility as the degree of bend in the smaller proximal thoracic curve just above the endplate of the fusion. This curve typically forms to compensate for the scoliotic main thoracic curve. The less flexible the compensatory curve pre-operatively, the less likely it is to assume a straighter position following surgery.
The upper-instrumented vertebra tilt anglerefers to the post-surgery angle at the top of the instrumented vertebra, below the compensatory curve. If the surgeon created a perfectly corrected main curve, tilt would be zero.
Resounding Affirmation
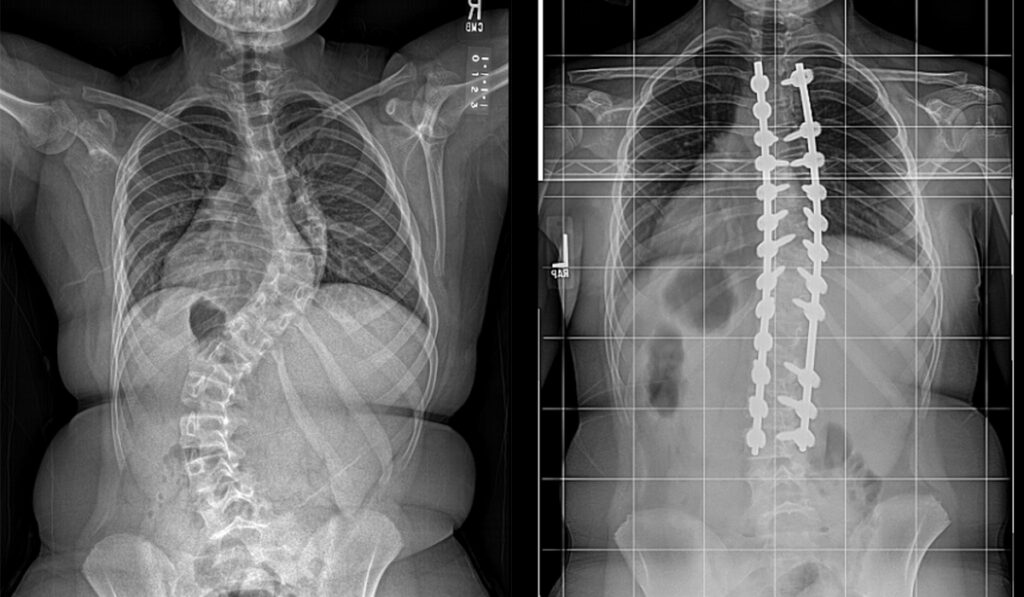
Louer’s team examined pre- and post-surgery radiographs from 161 adolescents who underwent posterior instrumented correction for thoracic-only curves.
He looked at both the flexibility of the proximal curve and the vertebral tilt and found that flexibility-tilt agreement was strongly associated with normal shoulder height, defined as no greater than a 5-degree difference between right and left shoulders.
Flexibility-tilt differences were found ranging from below 5 degrees to a greater than a 5-degree angle – independent of upper instrumented vertebra tilt – had been achieved in nearly half of the 74 patients (46 percent). This compares a mean proximal thoracic curve of between 7 and 19 degrees and a mean flexibility tilt difference of 1 to 13 degrees in this population overall.
Of the patients whose surgeries followed the flexibility-tilt agreement model, 83.8 percent achieved medial shoulder balance as a result. Just shy of 65 percent had achieved lateral shoulder balance at their most recent clinical follow-up.
Louer’s investigation showed that flexibility-tilt agreement was the strongest predictor of final medial and lateral shoulder balance for patients scoring 1 and 2 on the Lenke scoliosis classification scale.
“But patients with Lenke 1 curves and less stiff proximal curves, pre-operatively, were more likely to achieve agreement, ”Louer said.
In the OR
Louer says that some upper instrumented vertebra tilt is required to reach flexibility-tilt agreement in both curve types. The goal is to calculate flexibility preoperatively in order to achieve the desired tilt. The Receiving Operator Characteristic analysis showed that a difference of more than 5 degrees creates the imbalance, he said.
“But if you’re within 5 degrees, it’s going to be a pretty good outcome, ”Louer said.
Fusion Height in Debate
In a related study using the same patient data, Louer and his colleagues challenged the rule that fusions of the main thoracic curve should extend to T2-T4 to optimize correction and shoulder balance. They found that selecting an upper instrumented vertebra tilt of T5 or T6 in this population can achieve a comparable shoulder balance in properly selected patients.
“Most of us were trained that if the left shoulder is high pre-operatively, we fuse to T2,” Louer said.
“If the shoulders are level, you would go to T3, and if the right shoulder is higher, you would go to T4.
“Our conclusion from this study is that you can stop as low as T6 and still have a really good outcome if you get flexibility-tilt agreement, particularly with the less severe deformities.”
All Comers
Louer says that taking the flexibility-tilt agreement beyond Lemke 1 and 2 curves, and beyond adolescent patients is logically sound.
“I generally apply the concept to almost anyone who we can get a pre-operative flexibility film on,” he said. “It helps you avoid higher fusions that bring on extra risks of morbidity.”