No real treatment options existed for patients with severe chronic obstructive pulmonary disease until lung volume reduction surgery became widespread more than two decades ago.
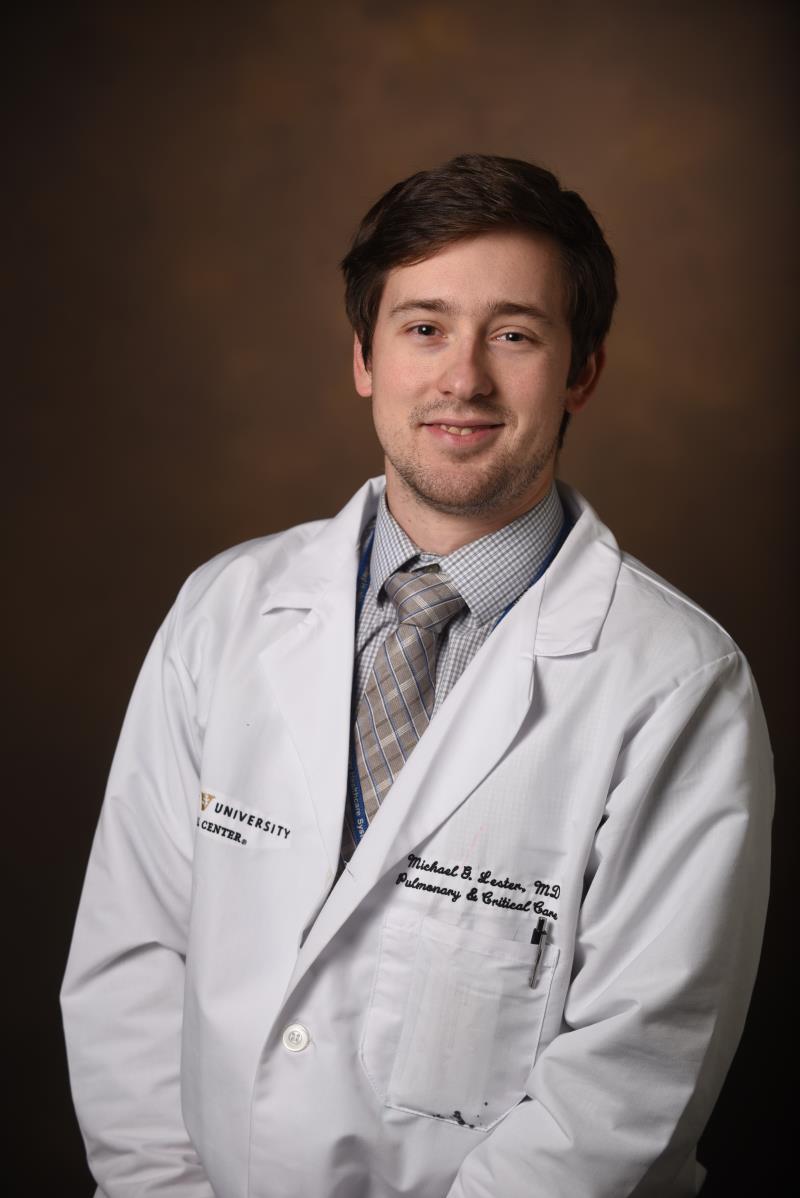
“For years we had bronchodilator inhalers, and that’s kind of where the treatment stopped,” said Michael G. Lester, MD, an assistant professor in the Division of Allergy, Pulmonary and Critical Care Medicine at Vanderbilt University Medical Center. “Eventually, people would progress to a point where these weren’t helping, and that’s about all we could do for them.”
“There are some promising new treatments, and we want to be at the forefront.”
Lester is clinical director of the Vanderbilt Lung Institute’s program for advanced COPD management, which offers those struggling with late-stage COPD a more comprehensive approach to care, including leading-edge imaging, as well as surgical and therapeutic approaches.
A key reason for establishing the program, Lester says, is to set up the pathways and infrastructure to support research into advanced COPD, especially through clinical trials.
“There are some promising new treatments, and we want to be at the forefront,” he added.
Early COPD Diagnosis
One area of research is X-ray velocimetry, a fluoroscopy-based imaging technique, to determine if it can be used to assess ventilation abnormalities that do not appear through standard testing methods.
A study presented at the 2023 American Thoracic Society International Conference evaluated XV in its assessment of specific ventilation abnormalities in Iraq and Afghanistan conflict veterans exposed to burn pits. The patients had been diagnosed with deployment-related constrictive bronchiolitis, yet many had normal pulmonary function tests and chest CT scans compared with healthy adults.
The fluoroscopy technique was shown to be a viable technique for assessing ventilation in this veteran cohort.
In another recent study, Lester and colleagues compared XV and pitot tube-assisted measures of ventilation in healthy adults. XV demonstrated a high degree of correlation with pitot tube parameters during tidal breathing and with bilevel-assisted breathing in healthy adults.
“XV is a promising tool to help us diagnosis COPD,” Lester said. “If XV could be used to confirm the regional distribution of ventilation, it would provide information that goes beyond the scope of conventional pulmonary testing or scans.”
Repairing Lung Mechanisms
Limited airflow caused by inflammation of the small airways and destruction of lung parenchyma can be the result of liminal narrowing and mucus production.
While LVRS can help improve airflow, it has its disadvantages, Lester said.
“There is a 4% mortality rate, it takes a while to recover, and if you don’t feel better, we can’t reverse it.”
A newer procedure, bronchoscopic LVRS, uses video-assisted placement of an endobronchial valve (Zephyr) to achieve similar benefits to conventional resection.
“Mortality is still 3%; but the endobronchial valve can be retrieved if it doesn’t work,” Lester explained. “In the right people, this approach can really make a difference.”
Lester says the procedure requires specialized knowledge in patient targeting and workup, as well as the skills of expert interventional pulmonologists who are trained to place the endobronchial valve.
“We are really fortunate to have good interventional background and the institutional support to spend time investigating these procedures,” he said.
Vanderbilt investigators are also recruiting for the multicenter RheSolve trial – a pivotal study to assess the safety and effectiveness of bronchial rheoplasty, which uses a balloon mechanism to deliver short bursts of high-frequency electrical energy to the airway epithelium.
Preclinical studies of rheoplasty have demonstrated regeneration of normalized epithelium following epithelial ablation.
Lester hopes to participate in an upcoming international study of targeted lung denervation, a novel bronchoscopic treatment aimed at disrupting peribronchial vagal innervation of the lung. Radiofrequency energy is delivered via a double-cooled catheter to ablate a narrow band around the main bronchi, while minimizing the effect to the inner surface of the airway.
Beyond Procedures
In addition to studies of interventional procedures, Lester has brought several clinical trials to Vanderbilt to ensure that COPD patients have access to cutting edge therapeutics, including anti-interleukin 33 monoclonal antibodies.
“The more treatments we have to offer, the better,” he said. “Unfortunately, we don’t have anything right now to stop disease progression. Our goal is to find long-term, durable options for preserving quality of life for all COPD patients.”