Vanderbilt University Medical Center researchers have found that care fragmentation is a key factor leading to greater polypharmacy – and a higher risk of medication-history errors.
The study, published recently in the Journal of the American Geriatrics Society, examined elements of Best Possible Medication History (BPMH) and was part of the recently completed Shed-MEDS deprescribing intervention for older adults with polypharmacy, which is generally described as someone regularly taking five or more medicines.
A Thorough Medication History
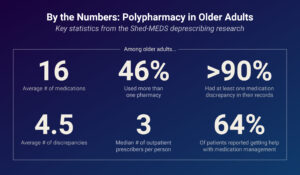
Obtaining an accurate, up-to-date list for polypharmacy patients can be challenging. In the study, the average participant was taking 16 medications. Vanderbilt researchers sought to incorporate gold-standard sources to obtain a detailed medical history, as well as to identify and quantify discrepancies in existing medication data.
“We went to all sources: we talked to the patients, we called all the pharmacies, and we used Tennessee’s Controlled Substance Monitoring Database, along with any existing medical records, to assemble the BPMH documentation,” said the study’s co-principal investigator, Eduard Vasilevskis, M.D., an associate professor of medicine at Vanderbilt.
While this degree of thoroughness is often not available in clinical practice, it allowed the team to define the issues more precisely.
Polypharmacy and Poly-Prescribing
Study participants were 372 hospital patients transitioning to post-acute care in a rehab or skilled-nursing facility. They were ages 69-85, mostly female (62 percent), white (84 percent), and all were multimorbid. Taking the pre-admission medication list as a starting point, researchers compared it with additional information from the patient, pharmacies and other sources. Discrepancies were categorized as medication omissions, additions, or errors in dosage.
“With multiple insurances and multiple co-pays, patients will seek the lowest cost.”
Over 90 percent of patients had at least one discrepancy in their records. The average number of discrepancies was 4.5. Categories with the highest number of discrepancies, in order of frequency, were blood pressure medications; over the counter, non-opioid analgesics such as NSAIDS; anti-cholinergics, including some over-the-counter drugs; and opioids.
Forty-six percent of patients received medications from more than one pharmacy, including internet and mail order services. The median number of outpatient prescribers was three.
“There are a lot of poly-prescribers and a lot of poly-pharmacies,” Vasilevskis said. “There are benefits of sub-specialized care, but a downside is fragmentation of care. With multiple insurances and multiple co-pays, patients will seek the lowest cost.”
He says the complexity of sourcing is directly related to more discrepancies in the medication history.
Technicians and Tech Offer Solutions
In looking at potential solutions supported by the study, Vasilevskis points to the field of dedicated pharmacy technicians – especially those caring for older, frailer patients. He also suggests more intentional data-sharing between pharmacies and health care institutions.
“More can be done to highlight the value and ROI of pharmacy technicians in patient care.”
“We’re fortunate at Vanderbilt to have a robust pharmacy department and the use of pharmacy technicians – but this is not always the case nationally,” he said. “More can be done to highlight the value and ROI of pharmacy technicians in patient care.”
Vasilevskis also emphasized the importance of patient empowerment.
“Patients are our best copilots for safety and quality.”
“Patients are our best copilots for safety and quality,” he said.
Improving and increasing the use of the personalized health record, such as MyHealth at Vanderbilt, can also make information portable and accessible to clinicians, care partners and health care systems.
“Sixty-four percent of our patients got some type of help with their medication. Making sure that the personalized health record is set up to engage the care partners, as well, is very important.”
Deprescribing In Practice
The next step, according to Vasilevskis, is to highlight the and medication discrepancies in older patients. Not everyone needs the level of BPMH applied in the study. Identifying which populations will benefit from the approach, and then ensuring that they get this intervention, will be key to future studies and in practice, the investigators said.
“How do we make deprescribing more pragmatic within the regular health operating system?”
In addition, resources like Tennessee’s Controlled Substance Monitoring Database, specific to opiates and benzodiazepines, could serve as an information-sharing template for all prescribed medicines.
“We just completed Shed-MEDS and published the final trial. What we did here can serve as a gold standard efficacy study – we looked under every rock to find medication omissions, discrepancies, and additions. That’s not going to be possible in every case. How do we make deprescribing more pragmatic within the regular health operating system?”




