A research team at Vanderbilt University Medical Center has completed initial testing of a model that uses non-invasive biomarkers to predict who is and is not likely to have lung cancer.
Eric Grogan, M.D., a thoracic surgeon and scientist at Vanderbilt, serves as principal investigator for the grant that funded the study. The trial results were published in the American Journal of Respiratory and Critical Care Medicine.
This work is part of the Vanderbilt-Ingram Cancer Center‘s multipronged effort to improve early detection of high-risk lung nodules and avoid unnecessary invasive procedures.
“Through this trial of our combined biomarker model, we found that about one in eight patients who don’t have cancer could avoid an unnecessary invasive procedure,” Grogan said. “We also found that we could significantly shorten time to diagnosis in those who do have cancer.”
First author Michael Kammer, Ph.D., a post-doctoral fellow in pulmonary medicine at Vanderbilt, highlights convenience and ease for the patient in using this combined biomarker model.
“One of the beauties of this trial is that there aren’t any extra procedures, exposures or costs to the patient to be able to do this, since they are already getting a blood draw and already have a CT scan,” Kammer said.
Screening Gaps and Confounders
While screening for early lung cancer is increasingly in the spotlight, most efforts remain laser-focused on people with a heavy smoking history.
“We found that about one in eight patients who don’t have cancer could avoid an unnecessary invasive procedure.”
“The rates of screening and positive survival outcomes are still absolutely abysmal,” Kammer said. “The guidelines screen in only a quarter of all people who get lung cancer. Further, only about five percent who are eligible get screened.”
Further complicating the diagnosis is a plethora of benign lung nodules.
“Biopsy is the only means to definitive diagnosis, yet there are costs and risks with bronchoscopy or needle biopsy, particularly in peripherally located nodules, where the risk of a collapsed lung is about 20 percent,” Kammer added.
“Nodules are so frequently observed incidentally on scans that unless the patient is a smoker and has personal or family history of cancer, the patient may be sent home for six months.
“Currently, the risks in getting a biopsy may not be considered justifiable by the fact that only about five percent of nodules turn out to be malignant. But those five percent can be aggressive, and six months later can be too late.”
New Predictive Model
Recognizing these shortfalls, the late Pierre Massion, M.D.*, former director of the Cancer Early Detection and Prevention Initiative at Vanderbilt, and his team came up with a three-way approach for refining the criteria for nodule testing: radiomics, expanded clinical history and a biomarker blood test.
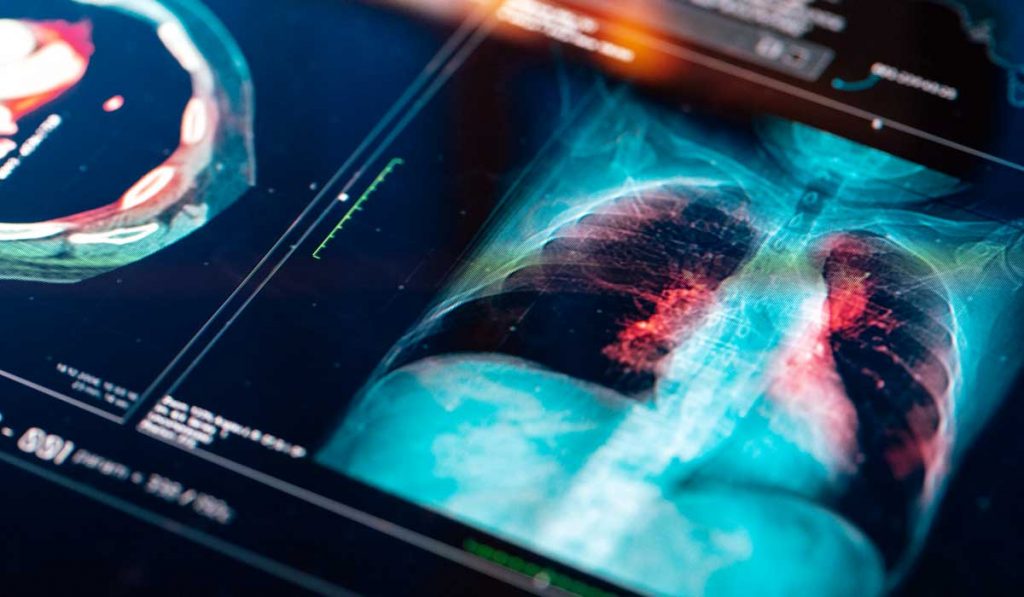
Through quantitative radiomics, a software algorithm analyzes an original CT scan for 750 quantitative features of the nodule.
“Currently, clinicians look primarily at size and shape, spiculation and lobulation to inform their next step,” Kammer said. “This looks at a myriad of feature subsets, as well as volume, density, heterogeneity and more.”
The second leg of the tripod is expanded clinical history, which includes the patient’s age, smoking history, family history and history of any other cancers, since all four have strong correlations with lung cancer risk.
“The risks in getting a biopsy may not be considered justifiable by the fact that only about five percent of nodules turn out to be malignant. But those five percent can be aggressive.”
A new test for CYFRA 21-1, a cytokeratin fragment and circulating biomarker, is based upon a new technology developed at Vanderbilt by Kammer and Darryl J. Bornhop, Ph.D., and provides the novel third leg of the tripod. Fragments of CYFRA 21-1 from lung epithelial cells are discarded into the bloodstream in higher quantities in the presence of infection, COPD, asthma or lung cancer, Kammer said.
“Together with the other parameters in the testing, it’s a significant biomarker.”
Combined Biomarker Outcomes
In their recent trial, the team analyzed records from 456 patients who had a lung nodule detected incidentally on a CT scan and were at intermediate risk for lung cancer, per published standards. Risk was then assessed by the predictive model.
Their study revealed that a combined biomarker-guided strategy “would have reduced invasive procedures from 62.9 percent to 50.6 percent in the intermediate-risk benign population and shorten the median time to diagnosis of cancer from 60 to 21 days in intermediate-risk cancers,” the authors wrote.
Next up, the team is funded to test this approach prospectively at Vanderbilt or the trial’s sister site, the University of Colorado, over the next two years.
“The goal of this trial is to show that using a combination biomarker approach will decrease the time to lung cancer diagnosis while reducing invasive procedures,” Grogan said. “Our hope is to also continue adding or refining the specific biomarkers in future trials.”
*The team dedicates their work and this article to Pierre Massion, M.D. – our inspiration, mentor, teacher, counselor, colleague, friend, and guiding light. May we honor his legacy in our continued work to improve outcomes in lung cancer through our study of lung cancer development, biomarkers, and early detection. Every step forward will be taken down a path you have paved. May we always be inspired by patients, driven by science, and empowered by each other.