Acute kidney injury (AKI), defined as a sudden loss of kidney function, is on the rise, with some studies suggesting incidence up 10 percent per year across patient groups. While AKI was once considered a self-limiting condition, it’s now know to be associated with future loss of kidney function, cardiovascular disease, poor quality of life and higher mortality risk.
Unfortunately, improved understanding of AKI’s longer-term consequences may not have led to better recognition and education for patients leaving the hospital, according to new research. A study published in the March 2019 American Journal of Nephrology found that most patients were unaware they had suffered an AKI event.
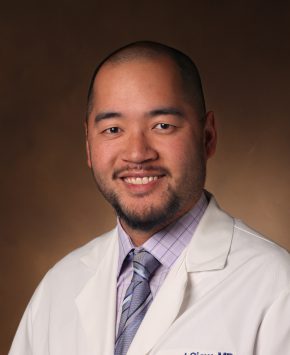
Edward Siew, M.D., associate professor of medicine in Vanderbilt University Medical Center’s Division of Nephrology and Hypertension, was lead author on the study. “These findings identify a strong opportunity to better inform patients about this condition. Ultimately, this may help them better engage in treatment plans centered around optimizing their long-term kidney health,” Siew said.
Measuring Patient Awareness
The researchers used a cross-sectional survey on AKI-related awareness and knowledge to sample patients who had suffered a Stage II or Stage III AKI event in Vanderbilt’s adult hospital near the time of their discharge. All 137 patients were asked to answer two key survey questions:
1. Did you experience acute kidney injury (AKI) while in the hospital?
2. Do you have a problem with your kidney health?
These questions were followed by a 15-item questionnaire on kidney knowledge.
Eighty percent of patients were unaware they had experienced AKI and 53 percent were unaware of either having AKI or a “problem with your kidney health.” Less than 50 percent were knowledgeable about AKI risks associated with NSAIDs and phosphate-based cathartics, and more than 80 percent said they desired more information about kidney care.
Kerri Cavanaugh, M.D., an associate professor of medicine in Vanderbilt’s Division of Nephrology and Hypertension, was the senior author on the study. “We found that when a patient is seen in outpatient follow-up and informed by their physician about AKI, they are often surprised by the diagnosis. This may contribute to patients’ reporting a poor experience of hospital care, and it identifies communication around the discharge transition as an important opportunity to improve quality of care,” Cavanaugh said.
In addition to being at higher risk for chronic kidney disease, patients who have experienced AKI may be more sensitive to future injury. Siew was an author on another study that showed nearly 20 percent of patients who previously experienced acute renal failure in the hospital regularly took NSAIDs—increasing AKI risk. Improving awareness of AKI and its risk factors might help patients reduce exposure to some of those risk factors.
“Understanding how knowledge or lack of it associates with future kidney outcomes, and whether improving knowledge can help improve long-term outcomes, are important future areas of study,” Siew said.
Improving Communication
In the hospital setting, communicating clearly and validating a patient’s understanding of AKI presents challenges. Chief among these are varying degrees of patient wakefulness/lucidity, the volume of activities that surround the discharge process, and the sheer number of issues the patient may have to comprehend throughout hospitalization. In addition, AKI most commonly occurs as a complication of another illness, so it may not be the main focus of communications.
Most cases of AKI in the hospital are managed without the need for a nephrologist. However, when patients had a nephrology consult (usually due to more severe AKI), they had a higher awareness of their AKI/kidney issues, even when the data were adjusted for the severity.
“It is our hope that physicians will introspect about what they can do… Everybody should be involved.”
“It is our hope that physicians will introspect about what they can do to eliminate this information gap,” Cavanaugh said. “Everybody should be involved and addressing this within their specific context of care and their expertise in the hospital stay continuum, with nephrology support as needed.”
Siew recently helped plan a National Institute of Diabetes and Digestive and Kidney Disease workshop, which incorporated patient representatives who had experienced severe AKI with prolonged recovery. “Patients didn’t necessary think they had an advocate there in the process. Clearly, there is more we can do to supply the information patients tell us they desire,” Siew said.