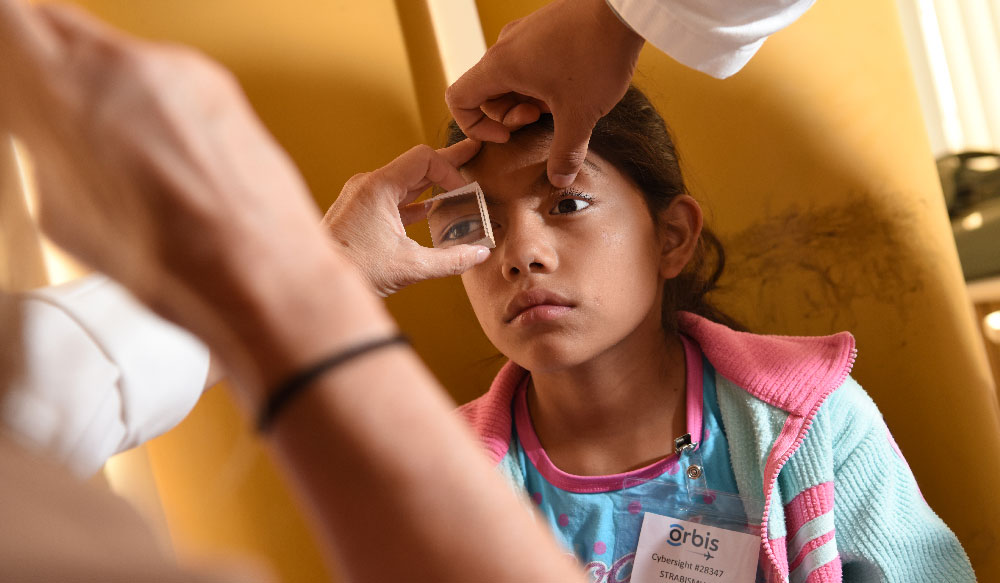
Not every young surgeon practices in a setting with mentorship from experienced faculty. At a teaching hospital in Trujillo, Peru, a new partnership between Orbis International and Vanderbilt Eye Institute is offering that mentorship remotely. Orbis, known for its flying hospital with multiple surgical suites and volunteer surgeons, is offering its telemedicine platform to connect experienced eye surgeons with junior faculty in Trujillo to improve cataract surgery skills.
Laura Wayman, M.D., vice chair of education for the Department of Ophthalmology and Visual Sciences at Vanderbilt, is the first surgeon to collaborate with Orbis as a mentor in the program.
“When Orbis first approached me at the International Council of Ophthalmology I was hesitant,” Wayman said. “What would happen if something went wrong and I wasn’t there to take over? But they have this amazing communications platform. Before anything happens in the operating room, there’s a lot of preparation.”
Remote Surgery with a View
One week in advance, the Peruvian surgeon sends Wayman patient information via Cybersight, Orbis’ telemedicine platform, including photos and lab work (patients are counseled regarding the surgery and tele-mentorship). The surgeon completes a standardized form outlining the surgical plan and Wayman evaluates whether the case is appropriate for remote guidance.
“First I ask them ‘What is your goal?’” Wayman explained. “Depending on the answer, I ask questions and provide feedback. It’s helpful to know if they want to perfect surgical skills or just improve efficiency.”
If she decides to proceed with the case, Wayman and the surgeon communicate via Cybersight prior to the surgery. On the day of surgery, the platform employs Zoom, the online video conferencing software, to bring the locations together. Testing is conducted with the local hospital’s IT team and with the mentor, and tech personnel are on hand during the procedure.
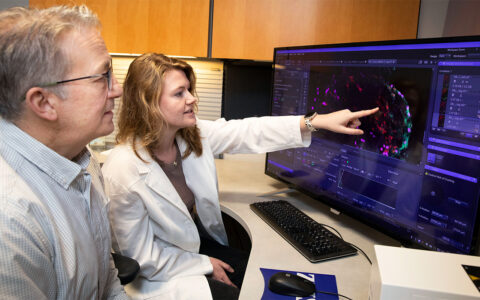
Once a connection is established via the secure interface, Wayman views the surgery through a specially designed camera connected to a microscope. Video quality is broadcast-grade, allowing her to clearly see anatomy and instrument manipulation. The surgeon wears an audio headset and hands-free mic, and the mentor can use headphones to streamline audio quality. For the surgeons, both audio and video latencies are well within margins of acceptability.
Post-surgery Feedback
Surgeons send Wayman post-op updates one day and one week after procedures and she provides timely feedback. From reports thus far, mentees have seamlessly integrated improved surgical techniques – showing measurable qualitative changes.
“It’s not like I’m teaching residents,” Wayman said. “These are people who’ve been operating, but they’re junior and trying to improve their skills. Once they’ve been in surgery on their own, they report back to me how often they’ve been able to reproduce what I taught them.”
What’s Next for Remote Mentorship?
Early outcomes suggest remote surgical mentorship across long distances is feasible for live microsurgery. “The problem,” Wayman said, “is finding people who are experienced in surgical instruction who want to be mentors. Then there are the language requirements.”
Wayman is fluent in Spanish and communicates with the Peruvian surgeons in their native language, which has proved more effective than speaking English. In addition to Spanish, the program is seeking mentors who speak Mandarin and Vietnamese.
“We’re not just training these surgeons,” said Wayman. “These individuals are in turn training residents; this is how the expansion will occur. This small region in South America is just the beginning.”