The National Lung Screening Trial (NLST), which included more than 50,000 participants, concluded that screening with the use of low-dose chest computed tomography (CT) detects lung tumors at early stages, when the cancer is curable, and reduces the risk of death. However, most patients today are still diagnosed at a late stage of the disease.
“Low-dose CT helps us save lives by decreasing the relative risk of lung cancer-specific mortality by 20 percent among high-risk persons,” said Pierre Massion, M.D., professor of Medicine and the director of the Cancer Early Detection and Prevention Initiative at Vanderbilt-Ingram Cancer Center, an NLST site. “The goal is to move the needle toward diagnosing people early, therefore offering them the opportunity for a true cure, typically with surgery.”
An Innovative Screening Program
“When the report came out in 2011 that the results of the trial were positive, we began collaborating with our radiology department to develop a lung cancer screening program,” said Massion. “Since 2015, when the Centers for Medicare and Medicaid Services approved national lung cancer screening as a covered benefit for people with Medicare, we’ve been able to ramp the program up.”
“So far, it has been extremely successful under the leadership of Dr. Kim Sandler. We’ve screened over 1,000 persons and identified over 30 lung cancers, the majority being stage 1.” Vanderbilt conducts the CT screenings at three different sites and is developing strategies to expand into the Vanderbilt Health network.
“As low-dose chest CT screening is being implemented, we diagnose many more lung nodules,” Massion said. “These require specific management. For patients with suspicious nodules, different strategies are offered based on risk and may include chest CT follow-up exam, a PET scan or a biopsy.”
”We’re looking at the benefits not just for lung health but for overall health.”
Massion hopes that the use of CT, combined with more sensitive screening tools, will help physicians quantify the risk for cardiovascular disease, osteoporosis, metabolism-related diseases such as diabetes, and even obesity-related cancers. “When you do a low-dose chest CT,” he explained, “you don’t just image the lungs. You also image the heart, esophagus, bones, fat and breasts. We’re looking at the benefits not just for lung health but for overall health.”
Molecular Lung Cancer Screening
In his research, Massion focuses on the development of molecular screening approaches to quantify the risk of lung cancer. He and his Vanderbilt research collaborators in pathology, molecular biology, biochemistry and biomedical engineering are using new methods to find genes, proteins or metabolites to identify molecular markers of disease risk.
“Now we are putting a lot of effort into identifying the 15 to 20 percent of people who are lifelong smokers who are at risk,” he said. “We think that there may be molecular predictors of cancer development in the airways of these individuals that can help us identify who is likely to develop lung cancer and offer them a surveillance program.”
In a 2016 study published in JCI Insight, Massion and co-investigators found risk-associated changes in the bronchial epithelium proteome driving changes in cellular metabolism that may offer new insights into the molecular pathogenesis of lung cancer. Results showed that the application of molecular biomarkers in the early detection of lung cancer may substantially improve the ability to select patients for lung cancer screening.
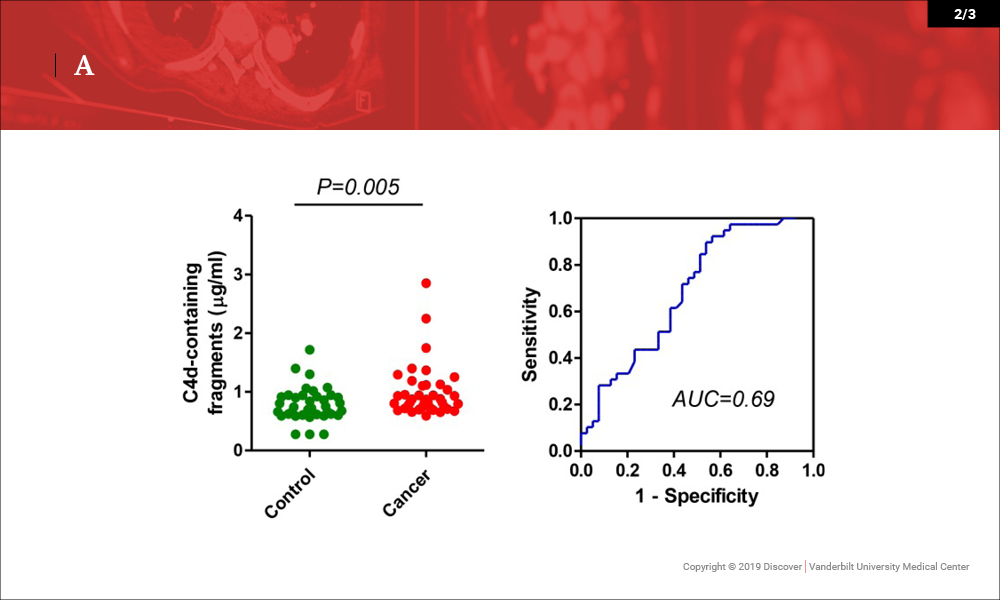
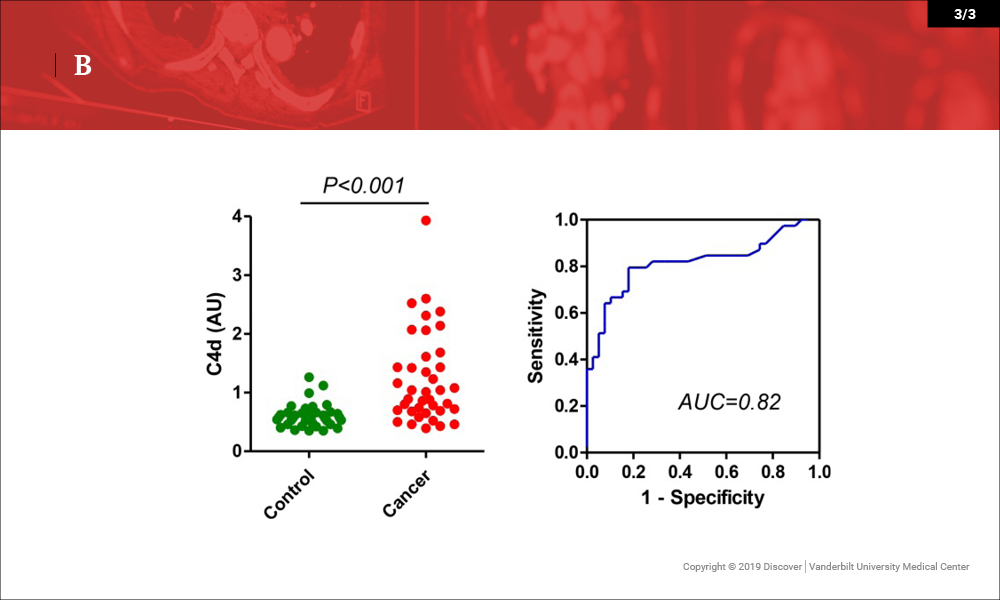
In a recent paper published in Oncotarget, the investigators reported that C4d-containing fragments of complement C4 are elevated in plasma and bronchoalveolar lavage samples from lung cancer patients, and may be of value for the diagnosis of the disease. This marker may also have diagnostic value in head and neck malignancies.
“I’m convinced that molecular tools have sensitivities and specificities needed to complement low-dose chest CT screening in ways that will better equip us to select high-risk individuals,” said Massion. “And once we are faced with lung nodules, if we can identify those who have a malignancy based on non-invasive methods such as circulating tumor DNA in the plasma, for example, we can reduce the resources required for diagnosis and accelerate their treatment.”