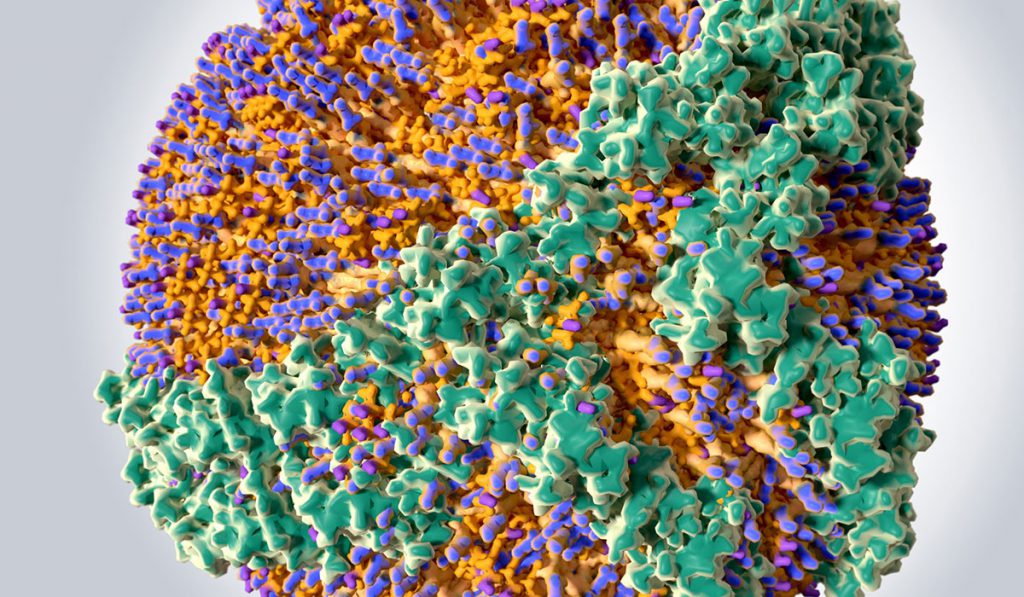
As advances are made in the understanding of how HDL functions in the kidneys, it is becoming increasingly clear that its role is much more complex than simply helping to reduce cholesterol levels.
Low levels of HDL have long been linked to lower risks for cardiovascular disease. A closer look reveals the specific type of HDL particle is what matters most, with certain particles activating detrimental pathways that can promote kidney damage.
A recently published review in the journal Pediatric Nephrology of the role kidneys play in HDL metabolism especially targets the main HDL protein, apolipoprotein AI (apoAI), and outlines how it can provide both positive and negative effects.
“This review outlines the idea that aside from albumin, filtered apoAI is a bioactive molecule that alters the phenotype of renal parenchymal cells, e.g., proliferation, synthesis of inflammatory/profibrotic factors that promote tubulointerstitial fibrosis,” said Valentina Kon, M.D., Margaret T. and H. Laird Smith Chair and professor of Pediatrics in Pediatric Nephrology at Vanderbilt University Medical Center.
While the role kidneys play in regulating HDL and its components has been studied in adults, there is a gap in the literature for how it relates to children. Further investigation could especially lead to discoveries that may help guide treatment of chronic kidney disease and other renal injuries.
The review, conducted by Pediatric Nephrologists working in Monroe Carell Jr. Children’s Hospital at Vanderbilt, targets apoAI/HDL as it has been shown to have a complex dual-sided role.
LipoprotEIns may become dysfunctional in kidney disease patients
“Our studies support that idea that disease such as kidney damage alters normally beneficial lipoproteins to become dysfunctional and actually propagate fibrotic injury.”
Study authors suggest that interactions between normal apoAI/HDL from the filtrate and kidney cells provide beneficial or protective effects. However, when modified apoAI/HDL is observed, as in the case of those with chronic kidney disease, the protein enhances the likelihood of harmful lipoproteins reaching the kidneys.
“Our studies support that idea that disease such as kidney damage alters normally beneficial lipoproteins to become dysfunctional and actually propagate fibrotic injury,” said Kon.
The most recent data reveals apoAI/HDL can affect lymphatic endothelial cells (LECs) and lymphatic vessels and may disrupt those vessels’ regulation of biologic processes.
Preliminary studies have shown apoAI can modify lymphangiogenesis either through its direct effect on LECs or by working through the interaction between LECs and tubular epithelial cells (TECs). The source for apoAI in the kidney is the glomerular ultrafiltrate, leading study authors to suggest urinary apoAI taken into the renal interstitial space can regulate the renal lymphatic network, which can have profound consequences.
“We suggest that tubular reabsorption of bioactive substances in the urine not only expand lymphatic vessel growth but also causes adverse remodeling of the lymphatic vascular network, inefficient interstitial clearance of edema/lipoproteins/bioactive molecules that contributes to progressive kidney damage,” said Kon.